User login
Challenges in Sports Medicine and Orthopedics
After playing football, an 18-year-old man presented to the ED with severe pain in his right arm. He stated that while throwing a pass, he felt a "snap" in his right arm and has been unable to move the arm since the injury. Radiographs were completed.
What is your interpretation of the radiographic image (Figure 1)?
Dr Patterson, editor of "Challenges in Sports Medicine and Orthopedics," is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
The radiograph (Figure 2) revealed a minimally displaced pathologic fracture (red arrow) through the midshaft of the humerus, which resulted from a space-occupying lesion (green arrow) in the humeral diaphysis. Since the radial nerve is commonly affected in this type of injury due to its close proximity to the humeral midshaft, careful neurologic assessment at the wrist and hand is essential. Injury to the nerve can occur during the fracture or reduction of the fracture, causing weakness in the extensors of the hand and numbness in the first dorsal web space. The incidence of radial nerve palsy in midshaft fractures of the humerus is 16%.1
In nondisplaced or minimally displaced fractures of the humeral midshaft, conservative management with a U-shaped (sugar-tong) splint from axilla to shoulder with elasticized wrap and sling is recommended. Surgical management is indicated in comminuted, significantly displaced, nonreducible, pathologic cases or in fractures resulting in neurovascular compromise. The patient in this case was referred to an orthopedic surgeon for open treatment.
- Smith WR, Agudelo JF, Parekh AA, Shank, JR. Musculoskeletal trauma surgery. In: Skinner HB, ed. Current Diagnosis & Treatment in Orthopedics. 4th ed. McGraw Hill Companies, Inc; 2006:121.
After playing football, an 18-year-old man presented to the ED with severe pain in his right arm. He stated that while throwing a pass, he felt a "snap" in his right arm and has been unable to move the arm since the injury. Radiographs were completed.
What is your interpretation of the radiographic image (Figure 1)?
Dr Patterson, editor of "Challenges in Sports Medicine and Orthopedics," is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
The radiograph (Figure 2) revealed a minimally displaced pathologic fracture (red arrow) through the midshaft of the humerus, which resulted from a space-occupying lesion (green arrow) in the humeral diaphysis. Since the radial nerve is commonly affected in this type of injury due to its close proximity to the humeral midshaft, careful neurologic assessment at the wrist and hand is essential. Injury to the nerve can occur during the fracture or reduction of the fracture, causing weakness in the extensors of the hand and numbness in the first dorsal web space. The incidence of radial nerve palsy in midshaft fractures of the humerus is 16%.1
In nondisplaced or minimally displaced fractures of the humeral midshaft, conservative management with a U-shaped (sugar-tong) splint from axilla to shoulder with elasticized wrap and sling is recommended. Surgical management is indicated in comminuted, significantly displaced, nonreducible, pathologic cases or in fractures resulting in neurovascular compromise. The patient in this case was referred to an orthopedic surgeon for open treatment.
After playing football, an 18-year-old man presented to the ED with severe pain in his right arm. He stated that while throwing a pass, he felt a "snap" in his right arm and has been unable to move the arm since the injury. Radiographs were completed.
What is your interpretation of the radiographic image (Figure 1)?
Dr Patterson, editor of "Challenges in Sports Medicine and Orthopedics," is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
The radiograph (Figure 2) revealed a minimally displaced pathologic fracture (red arrow) through the midshaft of the humerus, which resulted from a space-occupying lesion (green arrow) in the humeral diaphysis. Since the radial nerve is commonly affected in this type of injury due to its close proximity to the humeral midshaft, careful neurologic assessment at the wrist and hand is essential. Injury to the nerve can occur during the fracture or reduction of the fracture, causing weakness in the extensors of the hand and numbness in the first dorsal web space. The incidence of radial nerve palsy in midshaft fractures of the humerus is 16%.1
In nondisplaced or minimally displaced fractures of the humeral midshaft, conservative management with a U-shaped (sugar-tong) splint from axilla to shoulder with elasticized wrap and sling is recommended. Surgical management is indicated in comminuted, significantly displaced, nonreducible, pathologic cases or in fractures resulting in neurovascular compromise. The patient in this case was referred to an orthopedic surgeon for open treatment.
- Smith WR, Agudelo JF, Parekh AA, Shank, JR. Musculoskeletal trauma surgery. In: Skinner HB, ed. Current Diagnosis & Treatment in Orthopedics. 4th ed. McGraw Hill Companies, Inc; 2006:121.
- Smith WR, Agudelo JF, Parekh AA, Shank, JR. Musculoskeletal trauma surgery. In: Skinner HB, ed. Current Diagnosis & Treatment in Orthopedics. 4th ed. McGraw Hill Companies, Inc; 2006:121.
Severe Left Shoulder Pain After a Fall
Corticosteroid Injections May Help Injured NFL Players Return to Play Sooner
Corticosteroid injections may hasten the return time for National Football League (NFL) players suffering from high ankle sprains, according to research presented by Alfred A. Mansour, MD, from UT-Houston Health Sciences Center in Houston, Texas and colleagues. Treatment methods were not well documented in the literature. These stable syndesmosis ankle sprains are common in athletes that participate in contact sports. Standard radiographs and magnetic resonance imaging (MRI) were used to confirm the players’ diagnoses. All injuries confirmed with MRI were reviewed. Combining the corticosteroid and rehabilitation, those 13 players (Group 1) treated with these injections typically returned to play 40% sooner than those, 18 players (Group 2), not receiving the same corticosteroid injection. For these 13 players it was a return-to-play approximately 10 days sooner.
Syndesmosis sprains require more treatment as well as more time off from play (ie, games and practice) for recovery as compared to lateral ankle sprains. “After examining players with stable high ankle sprains over an eight-year period, we discovered those treated with corticosteroid injections returned to play within an average 15 days, as compared to 25 days for those not treated similarly,” noted Mansour. The players were examined between the years 2003 and 2011. “For high-level athletes such as NFL players, returning to play 10 days sooner can have a significant impact personally and for the team,” added Mansour as syndesmosis sprain injuries result in significant time lost from playing in both practice and games.
The study examined 31 players from two NFL teams, with Group 1 (13 players) receiving a corticosteroid injection within 72 hours of an ankle injury. Group 2 (18 players) did not receive the corticosteroid injection. All players involved in the study went through a standard nonoperative rehabilitation program, including: crutches, weight-bearing activity as tolerated, nonsteroidal anti-inflammatory drugs (NSAIDs) treatment, and a progressive return-to-play training based on the treatment practices of the respective team. The difference in return-to-play was statistically significant (p=0.0097).
“While previous research explores the extended recovery involved with these injuries, our data offers a new treatment option that may be more effective for NFL players,” noted Mansour. “Further research can help confirm this, though we are excited to discover ways to help athletes at the professional level,” Mansour continued.
Mansour and colleagues reported no complications in players treated with the corticosteroid injections. In a highly competitive athlete, the ability to return-to-play sooner rather than later may represent a significant clinical difference.
Corticosteroid injections may hasten the return time for National Football League (NFL) players suffering from high ankle sprains, according to research presented by Alfred A. Mansour, MD, from UT-Houston Health Sciences Center in Houston, Texas and colleagues. Treatment methods were not well documented in the literature. These stable syndesmosis ankle sprains are common in athletes that participate in contact sports. Standard radiographs and magnetic resonance imaging (MRI) were used to confirm the players’ diagnoses. All injuries confirmed with MRI were reviewed. Combining the corticosteroid and rehabilitation, those 13 players (Group 1) treated with these injections typically returned to play 40% sooner than those, 18 players (Group 2), not receiving the same corticosteroid injection. For these 13 players it was a return-to-play approximately 10 days sooner.
Syndesmosis sprains require more treatment as well as more time off from play (ie, games and practice) for recovery as compared to lateral ankle sprains. “After examining players with stable high ankle sprains over an eight-year period, we discovered those treated with corticosteroid injections returned to play within an average 15 days, as compared to 25 days for those not treated similarly,” noted Mansour. The players were examined between the years 2003 and 2011. “For high-level athletes such as NFL players, returning to play 10 days sooner can have a significant impact personally and for the team,” added Mansour as syndesmosis sprain injuries result in significant time lost from playing in both practice and games.
The study examined 31 players from two NFL teams, with Group 1 (13 players) receiving a corticosteroid injection within 72 hours of an ankle injury. Group 2 (18 players) did not receive the corticosteroid injection. All players involved in the study went through a standard nonoperative rehabilitation program, including: crutches, weight-bearing activity as tolerated, nonsteroidal anti-inflammatory drugs (NSAIDs) treatment, and a progressive return-to-play training based on the treatment practices of the respective team. The difference in return-to-play was statistically significant (p=0.0097).
“While previous research explores the extended recovery involved with these injuries, our data offers a new treatment option that may be more effective for NFL players,” noted Mansour. “Further research can help confirm this, though we are excited to discover ways to help athletes at the professional level,” Mansour continued.
Mansour and colleagues reported no complications in players treated with the corticosteroid injections. In a highly competitive athlete, the ability to return-to-play sooner rather than later may represent a significant clinical difference.
Corticosteroid injections may hasten the return time for National Football League (NFL) players suffering from high ankle sprains, according to research presented by Alfred A. Mansour, MD, from UT-Houston Health Sciences Center in Houston, Texas and colleagues. Treatment methods were not well documented in the literature. These stable syndesmosis ankle sprains are common in athletes that participate in contact sports. Standard radiographs and magnetic resonance imaging (MRI) were used to confirm the players’ diagnoses. All injuries confirmed with MRI were reviewed. Combining the corticosteroid and rehabilitation, those 13 players (Group 1) treated with these injections typically returned to play 40% sooner than those, 18 players (Group 2), not receiving the same corticosteroid injection. For these 13 players it was a return-to-play approximately 10 days sooner.
Syndesmosis sprains require more treatment as well as more time off from play (ie, games and practice) for recovery as compared to lateral ankle sprains. “After examining players with stable high ankle sprains over an eight-year period, we discovered those treated with corticosteroid injections returned to play within an average 15 days, as compared to 25 days for those not treated similarly,” noted Mansour. The players were examined between the years 2003 and 2011. “For high-level athletes such as NFL players, returning to play 10 days sooner can have a significant impact personally and for the team,” added Mansour as syndesmosis sprain injuries result in significant time lost from playing in both practice and games.
The study examined 31 players from two NFL teams, with Group 1 (13 players) receiving a corticosteroid injection within 72 hours of an ankle injury. Group 2 (18 players) did not receive the corticosteroid injection. All players involved in the study went through a standard nonoperative rehabilitation program, including: crutches, weight-bearing activity as tolerated, nonsteroidal anti-inflammatory drugs (NSAIDs) treatment, and a progressive return-to-play training based on the treatment practices of the respective team. The difference in return-to-play was statistically significant (p=0.0097).
“While previous research explores the extended recovery involved with these injuries, our data offers a new treatment option that may be more effective for NFL players,” noted Mansour. “Further research can help confirm this, though we are excited to discover ways to help athletes at the professional level,” Mansour continued.
Mansour and colleagues reported no complications in players treated with the corticosteroid injections. In a highly competitive athlete, the ability to return-to-play sooner rather than later may represent a significant clinical difference.
Shoulder Surgery May Make Sense for Young Patients
Arthroscopic bankart repair surgery is a costeffective alternative approach for patients suffering their first anterior shoulder dislocation, according to research presented by Ryan Patrick Donegan, MD, from Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, and colleagues based on using currently available probabilities, estimated costs, and prospectively collected health state utilities.
“We based our conclusions on a Markov model, which takes into account how surgery affects the patient’s recovery in relation to the actual costs of medical treatment,” commented Donegan. The incremental cost-effectiveness ratio (ICER) for arthroscopic bankart versus nonoperative treatment was approximately $43,500. “For surgery to be costeffective in this model, expenses must be under $24,457, the probability of re-dislocation must be under 7%, and the quality of life rating must not fall below 0.86,” Donegan noted. “Our research showed surgical costs of $11,267, probability of re-dislocation at only 4% and quality of life rating of 0.93—numbers suggesting surgery is a good investment for these patients,” continued Donegan. Therefore, the estimated cost of surgical treatment must increase from approximately $11,000 to $24,000 for surgery to no longer be cost-effective. The probability of nonoperative treatment must decrease from 17% to approximately 11% for surgery to also no longer be cost-effective.
Researchers drew data from literature reporting on first-time shoulder-repair arthroscopies in patients from 15 to 35 years old. They also gathered information from a 50-patient survey using a time trade-off method approved by the Dartmouth-Hitchcock Medical Center’s Institutional Review Board. The probabilities of the various treatment outcomes and the costs
associated with treatment were derived from the orthopaedic literature and adjusted Medicare reimbursement rates.
“Shoulder dislocations are one of the most common orthopaedic issues today, and our research shows that–after weighing all the options–surgery can be both helpful to the recovery process and cost-effective,” Donegan shared.
Donegan and colleagues note that nonoperative treatment based on rest and physical therapy should still be considered an effective treatment option for patients. There is still room for further studies to focus on identifying patient populations that fall within the threshold values identified in the analysis.
Arthroscopic bankart repair surgery is a costeffective alternative approach for patients suffering their first anterior shoulder dislocation, according to research presented by Ryan Patrick Donegan, MD, from Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, and colleagues based on using currently available probabilities, estimated costs, and prospectively collected health state utilities.
“We based our conclusions on a Markov model, which takes into account how surgery affects the patient’s recovery in relation to the actual costs of medical treatment,” commented Donegan. The incremental cost-effectiveness ratio (ICER) for arthroscopic bankart versus nonoperative treatment was approximately $43,500. “For surgery to be costeffective in this model, expenses must be under $24,457, the probability of re-dislocation must be under 7%, and the quality of life rating must not fall below 0.86,” Donegan noted. “Our research showed surgical costs of $11,267, probability of re-dislocation at only 4% and quality of life rating of 0.93—numbers suggesting surgery is a good investment for these patients,” continued Donegan. Therefore, the estimated cost of surgical treatment must increase from approximately $11,000 to $24,000 for surgery to no longer be cost-effective. The probability of nonoperative treatment must decrease from 17% to approximately 11% for surgery to also no longer be cost-effective.
Researchers drew data from literature reporting on first-time shoulder-repair arthroscopies in patients from 15 to 35 years old. They also gathered information from a 50-patient survey using a time trade-off method approved by the Dartmouth-Hitchcock Medical Center’s Institutional Review Board. The probabilities of the various treatment outcomes and the costs
associated with treatment were derived from the orthopaedic literature and adjusted Medicare reimbursement rates.
“Shoulder dislocations are one of the most common orthopaedic issues today, and our research shows that–after weighing all the options–surgery can be both helpful to the recovery process and cost-effective,” Donegan shared.
Donegan and colleagues note that nonoperative treatment based on rest and physical therapy should still be considered an effective treatment option for patients. There is still room for further studies to focus on identifying patient populations that fall within the threshold values identified in the analysis.
Arthroscopic bankart repair surgery is a costeffective alternative approach for patients suffering their first anterior shoulder dislocation, according to research presented by Ryan Patrick Donegan, MD, from Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, and colleagues based on using currently available probabilities, estimated costs, and prospectively collected health state utilities.
“We based our conclusions on a Markov model, which takes into account how surgery affects the patient’s recovery in relation to the actual costs of medical treatment,” commented Donegan. The incremental cost-effectiveness ratio (ICER) for arthroscopic bankart versus nonoperative treatment was approximately $43,500. “For surgery to be costeffective in this model, expenses must be under $24,457, the probability of re-dislocation must be under 7%, and the quality of life rating must not fall below 0.86,” Donegan noted. “Our research showed surgical costs of $11,267, probability of re-dislocation at only 4% and quality of life rating of 0.93—numbers suggesting surgery is a good investment for these patients,” continued Donegan. Therefore, the estimated cost of surgical treatment must increase from approximately $11,000 to $24,000 for surgery to no longer be cost-effective. The probability of nonoperative treatment must decrease from 17% to approximately 11% for surgery to also no longer be cost-effective.
Researchers drew data from literature reporting on first-time shoulder-repair arthroscopies in patients from 15 to 35 years old. They also gathered information from a 50-patient survey using a time trade-off method approved by the Dartmouth-Hitchcock Medical Center’s Institutional Review Board. The probabilities of the various treatment outcomes and the costs
associated with treatment were derived from the orthopaedic literature and adjusted Medicare reimbursement rates.
“Shoulder dislocations are one of the most common orthopaedic issues today, and our research shows that–after weighing all the options–surgery can be both helpful to the recovery process and cost-effective,” Donegan shared.
Donegan and colleagues note that nonoperative treatment based on rest and physical therapy should still be considered an effective treatment option for patients. There is still room for further studies to focus on identifying patient populations that fall within the threshold values identified in the analysis.
Range of Motion May be a Predictor for Elbow Injuries in Major League Baseball Pitchers
Certain elements of a pitcher’s throwing mechanics can increase the risk for elbow injuries, according to information presented by Kevin Wilk, DPT, from Champion Sports Medicine, in Birmingham, Alabama, and colleagues.
The researchers examined 296 Major League Baseball (MLB) pitchers throughout 8 seasons between 2005 and 2012. Pitchers with a deficit of more than five degrees in total range of motion (TRM) in their dominant shoulder had a 2.3 times higher risk of injury, while pitchers with a deficit of five or more degrees in shoulder flexion of the dominant shoulder had a 2.8 times higher risk of injury.
“Overhead throwing athletes like baseball pitchers are already prone to a unique set of elbow injuries,” included Dr. Wilk, who also noted, “with this in mind, we wanted to explore whether specific elements of the throwing motion can contribute to a greater injury risk.”
Patients’ passive range of motion (PROM) measurements for the study were assessed by clinicians with more than 35 years of experience, including 30 years of combined experience performing spring training physicals for professional baseball players. A bubble goniometer was used to assess PROM of both dominant and non-dominant shoulders. Of the 296 professional pitchers, 505 examinations were conducted. There was a significant impact on the risk of elbow injuries in pitchers with bilateral differences in total rotational motion.
“While we only identified 50 individual elbow injuries in this study, they resulted in an average of 51 days on the disabled list—or about one-fourth of a major league season,” contributed Wilk. “Hopefully our data can help team physicians and athletic trainers work to prevent these types of long-term injury absences,” noted Wilk.
Certain elements of a pitcher’s throwing mechanics can increase the risk for elbow injuries, according to information presented by Kevin Wilk, DPT, from Champion Sports Medicine, in Birmingham, Alabama, and colleagues.
The researchers examined 296 Major League Baseball (MLB) pitchers throughout 8 seasons between 2005 and 2012. Pitchers with a deficit of more than five degrees in total range of motion (TRM) in their dominant shoulder had a 2.3 times higher risk of injury, while pitchers with a deficit of five or more degrees in shoulder flexion of the dominant shoulder had a 2.8 times higher risk of injury.
“Overhead throwing athletes like baseball pitchers are already prone to a unique set of elbow injuries,” included Dr. Wilk, who also noted, “with this in mind, we wanted to explore whether specific elements of the throwing motion can contribute to a greater injury risk.”
Patients’ passive range of motion (PROM) measurements for the study were assessed by clinicians with more than 35 years of experience, including 30 years of combined experience performing spring training physicals for professional baseball players. A bubble goniometer was used to assess PROM of both dominant and non-dominant shoulders. Of the 296 professional pitchers, 505 examinations were conducted. There was a significant impact on the risk of elbow injuries in pitchers with bilateral differences in total rotational motion.
“While we only identified 50 individual elbow injuries in this study, they resulted in an average of 51 days on the disabled list—or about one-fourth of a major league season,” contributed Wilk. “Hopefully our data can help team physicians and athletic trainers work to prevent these types of long-term injury absences,” noted Wilk.
Certain elements of a pitcher’s throwing mechanics can increase the risk for elbow injuries, according to information presented by Kevin Wilk, DPT, from Champion Sports Medicine, in Birmingham, Alabama, and colleagues.
The researchers examined 296 Major League Baseball (MLB) pitchers throughout 8 seasons between 2005 and 2012. Pitchers with a deficit of more than five degrees in total range of motion (TRM) in their dominant shoulder had a 2.3 times higher risk of injury, while pitchers with a deficit of five or more degrees in shoulder flexion of the dominant shoulder had a 2.8 times higher risk of injury.
“Overhead throwing athletes like baseball pitchers are already prone to a unique set of elbow injuries,” included Dr. Wilk, who also noted, “with this in mind, we wanted to explore whether specific elements of the throwing motion can contribute to a greater injury risk.”
Patients’ passive range of motion (PROM) measurements for the study were assessed by clinicians with more than 35 years of experience, including 30 years of combined experience performing spring training physicals for professional baseball players. A bubble goniometer was used to assess PROM of both dominant and non-dominant shoulders. Of the 296 professional pitchers, 505 examinations were conducted. There was a significant impact on the risk of elbow injuries in pitchers with bilateral differences in total rotational motion.
“While we only identified 50 individual elbow injuries in this study, they resulted in an average of 51 days on the disabled list—or about one-fourth of a major league season,” contributed Wilk. “Hopefully our data can help team physicians and athletic trainers work to prevent these types of long-term injury absences,” noted Wilk.
Second ACL Injuries 6 Times More Likely After Reconstruction
Anterior cruciate ligament reconstruction (ACLR) surgery is a common knee injury procedure in the young active population, but the overall incidence of having to go through it again within 24 months is 6 times greater than someone who has never had an ACL tear, according to Mark V. Paterno, PhD, PT, ATC, from the Sports Medicine Biodynamics Center, Cincinnati, Ohio, and colleagues.
“In our study, female athletes after ACLR demonstrated more than 4 times greater rate of injury within 24 months than their healthy counterparts. This data highlights the fact that ACLR patients who return to playing sports are at greater risk for injury and should take appropriate precautions to prevent injury,” said Paterno.
Researchers analyzed data from 78 subjects (59 female, 19 male) between 10 and 25 years old, who underwent ACLR and were ready to return to a pivoting/cutting sport (RTS), and 47 healthy, control individuals. Each subject was followed for injury and athletic exposure for a 24-month period after returning to play. During that time 23 of the ACLR individuals and 4 control subjects suffered an ACL injury. Within the ACLR group, there also appeared to be a trend for female subjects to be 2 times more likely to suffer an injury on the opposite knee than on the previously injured one. Overall, 29.5% of athletes suffered a second ACL injury within 24 months of returning to activity with 20.5% sustaining an opposite leg injury and 9.0% incurring graft re-tear injury on the same leg. A higher proportion of females (23.7%) suffered an opposite leg injury compared to males (10.5%).
“Our study represents the first report of subsequent ACL injury incidence rate focused on 2-year outcomes of young, active patients returning to sport. Even though additional research still needs to be performed to support our findings, our data does provide early evidence for re-examining current rehabilitation and return to sport protocols following ACLR,” added Paterno.
Anterior cruciate ligament reconstruction (ACLR) surgery is a common knee injury procedure in the young active population, but the overall incidence of having to go through it again within 24 months is 6 times greater than someone who has never had an ACL tear, according to Mark V. Paterno, PhD, PT, ATC, from the Sports Medicine Biodynamics Center, Cincinnati, Ohio, and colleagues.
“In our study, female athletes after ACLR demonstrated more than 4 times greater rate of injury within 24 months than their healthy counterparts. This data highlights the fact that ACLR patients who return to playing sports are at greater risk for injury and should take appropriate precautions to prevent injury,” said Paterno.
Researchers analyzed data from 78 subjects (59 female, 19 male) between 10 and 25 years old, who underwent ACLR and were ready to return to a pivoting/cutting sport (RTS), and 47 healthy, control individuals. Each subject was followed for injury and athletic exposure for a 24-month period after returning to play. During that time 23 of the ACLR individuals and 4 control subjects suffered an ACL injury. Within the ACLR group, there also appeared to be a trend for female subjects to be 2 times more likely to suffer an injury on the opposite knee than on the previously injured one. Overall, 29.5% of athletes suffered a second ACL injury within 24 months of returning to activity with 20.5% sustaining an opposite leg injury and 9.0% incurring graft re-tear injury on the same leg. A higher proportion of females (23.7%) suffered an opposite leg injury compared to males (10.5%).
“Our study represents the first report of subsequent ACL injury incidence rate focused on 2-year outcomes of young, active patients returning to sport. Even though additional research still needs to be performed to support our findings, our data does provide early evidence for re-examining current rehabilitation and return to sport protocols following ACLR,” added Paterno.
Anterior cruciate ligament reconstruction (ACLR) surgery is a common knee injury procedure in the young active population, but the overall incidence of having to go through it again within 24 months is 6 times greater than someone who has never had an ACL tear, according to Mark V. Paterno, PhD, PT, ATC, from the Sports Medicine Biodynamics Center, Cincinnati, Ohio, and colleagues.
“In our study, female athletes after ACLR demonstrated more than 4 times greater rate of injury within 24 months than their healthy counterparts. This data highlights the fact that ACLR patients who return to playing sports are at greater risk for injury and should take appropriate precautions to prevent injury,” said Paterno.
Researchers analyzed data from 78 subjects (59 female, 19 male) between 10 and 25 years old, who underwent ACLR and were ready to return to a pivoting/cutting sport (RTS), and 47 healthy, control individuals. Each subject was followed for injury and athletic exposure for a 24-month period after returning to play. During that time 23 of the ACLR individuals and 4 control subjects suffered an ACL injury. Within the ACLR group, there also appeared to be a trend for female subjects to be 2 times more likely to suffer an injury on the opposite knee than on the previously injured one. Overall, 29.5% of athletes suffered a second ACL injury within 24 months of returning to activity with 20.5% sustaining an opposite leg injury and 9.0% incurring graft re-tear injury on the same leg. A higher proportion of females (23.7%) suffered an opposite leg injury compared to males (10.5%).
“Our study represents the first report of subsequent ACL injury incidence rate focused on 2-year outcomes of young, active patients returning to sport. Even though additional research still needs to be performed to support our findings, our data does provide early evidence for re-examining current rehabilitation and return to sport protocols following ACLR,” added Paterno.
Type of Helmet May Not Lower Concussion Risk
Approximately 40,000 high school football players get a concussion every year in the United States, but contrary to equipment manufacturers’ claims to lessen impact forces associated with sport related concussions (SRC), the specific brand of helmet and helmet age were not associated with lower risk of concussion, says Timothy McGuine, PhD, University of Wisconsin, Madison, Wisconsin, and colleagues.
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
Approximately 40,000 high school football players get a concussion every year in the United States, but contrary to equipment manufacturers’ claims to lessen impact forces associated with sport related concussions (SRC), the specific brand of helmet and helmet age were not associated with lower risk of concussion, says Timothy McGuine, PhD, University of Wisconsin, Madison, Wisconsin, and colleagues.
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
Approximately 40,000 high school football players get a concussion every year in the United States, but contrary to equipment manufacturers’ claims to lessen impact forces associated with sport related concussions (SRC), the specific brand of helmet and helmet age were not associated with lower risk of concussion, says Timothy McGuine, PhD, University of Wisconsin, Madison, Wisconsin, and colleagues.
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
Type of Helmet May Not Lower Concussion Risk
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
“According to our research, lower risks of sustaining a sports-related concussion (SRC) and its severity were not improved based on a specific manufacturer. In addition, the SRC rates were similar for players wearing new helmets, as compared to those wearing older ones,” commented McGuine. There is limited data detailing how specific types of football helmets and mouth guards affect the incidence and severity of SRC in players participating on high school football football teams. “It is also interesting to note, that players who wore a generic mouth guard provided by the school had a lower rate of SRC compared to players with more expensive mouth guards,” added McGuine.
Researchers collected data by Licensed Athletic Trainers (ATCs) at 36 public and private high schools in Wisconsin during the 2012 high school football season. A sample of 1,332 players were enrolled in the study with 251 (19%) individuals having reported at least 1 SRC within the last 6 years, and 171 (13%) players reporting 1 SRC within the previous 12 months. At each school the licensed athletic trainers recorded the brand, model, and purchase year of the helmets. They also recorded the type of mouth guard utilized (eg, generic, specialized or custom fit). Licensed athletic trainers also recorded the number and type of exposure (practice vs game) and the number of SRCs sustained. There were 115 (8.6%) players of the 1,332 that sustained 116 SRCs.
“Increased risk of concussions in our study was not associated with age, body mass index (BMI), grade in school, level of competition, or years of football experience. However, players with a history of SRC were twice as likely to sustain another one compared to players without a history. Additional screening to identify those players with increased concussion risk is a key to prevention and hopefully will help reduce rates in the future,” noted McGuine.
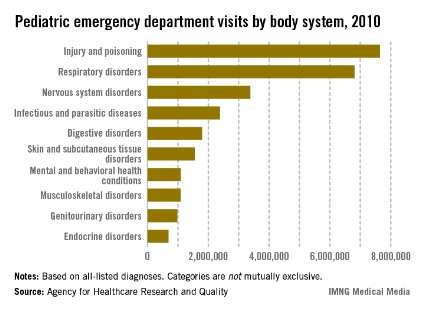
Injuries/poisonings the leading cause of pediatric ED visits
Injuries and poisonings were the most common reason for children to end up in the emergency department in 2010, accounting for over 7.6 million visits, the Agency for Healthcare Research and Quality reported.
There were a total of over 25.5 million ED visits by children under age 18 in 2010, with respiratory disorders being the second most common all-listed condition (6.8 million visits). The next most common reason was nervous system disorders (3.4 million visits), followed by infectious and parasitic diseases (2.4 million) and digestive disorders (1.8 million), according to the AHRQ.
Because the Healthcare Cost and Utilization Project – source of the AHRQ data – tracks all of a patient’s listed diagnoses, the body system categories are not mutually exclusive.
Injuries and poisonings were the most common reason for children to end up in the emergency department in 2010, accounting for over 7.6 million visits, the Agency for Healthcare Research and Quality reported.
There were a total of over 25.5 million ED visits by children under age 18 in 2010, with respiratory disorders being the second most common all-listed condition (6.8 million visits). The next most common reason was nervous system disorders (3.4 million visits), followed by infectious and parasitic diseases (2.4 million) and digestive disorders (1.8 million), according to the AHRQ.
Because the Healthcare Cost and Utilization Project – source of the AHRQ data – tracks all of a patient’s listed diagnoses, the body system categories are not mutually exclusive.
Injuries and poisonings were the most common reason for children to end up in the emergency department in 2010, accounting for over 7.6 million visits, the Agency for Healthcare Research and Quality reported.
There were a total of over 25.5 million ED visits by children under age 18 in 2010, with respiratory disorders being the second most common all-listed condition (6.8 million visits). The next most common reason was nervous system disorders (3.4 million visits), followed by infectious and parasitic diseases (2.4 million) and digestive disorders (1.8 million), according to the AHRQ.
Because the Healthcare Cost and Utilization Project – source of the AHRQ data – tracks all of a patient’s listed diagnoses, the body system categories are not mutually exclusive.