User login
Anti-Tumor Necrosis Factor Treatment for Glomerulopathy: Case Report and Review of Literature
Podocytes are terminally differentiated, highly specialized cells located in juxtaposition to the basement membrane over the abluminal surfaces of endothelial cells within the glomerular tuft. This triad structure is the site of the filtration barrier, which forms highly delicate and tightly regulated architecture to carry out the ultrafiltration function of the kidney.1 The filtration barrier is characterized by foot processes that are connected by specialized junctions called slit diaphragms.
Insults to components of the filtration barrier can initiate cascading events and perpetuate structural alterations that may eventually result in sclerotic changes.2 Common causes among children include minimal change disease (MCD) with the collapse of foot processes resulting in proteinuria, Alport syndrome due to mutation of collagen fibers within the basement membrane leading to hematuria and proteinuria, immune complex mediated nephropathy following common infections or autoimmune diseases, and focal segmental glomerulosclerosis (FSGS) that can show variable histopathology toward eventual glomerular scarring.3,4 These children often clinically have minimal, if any, signs of systemic inflammation.3-5 This has been a limiting factor for the commitment to immunomodulatory treatment, except for steroids for the treatment of MCD.6 Although prolonged steroid treatment may be efficacious, adverse effects are significant in a growing child. Alternative treatments, such as tacrolimus and rituximab have been suggested as second-line steroid-sparing agents.7,8 Not uncommonly, however, these cases are managed by supportive measures only during the progression of the natural course of the disease, which may eventually lead to renal failure, requiring transplant for survival.8,9
This case report highlights a child with a variant of uncertain significance (VUS) in genes involved in Alport syndrome and FSGS who developed an abrupt onset of proteinuria and hematuria after a respiratory illness. To our knowledge, he represents the youngest case demonstrating the benefit of targeted treatment against tumor necrosis factor-α (TNF-α) for glomerulopathy using biologic response modifiers.
Case Description
This is currently a 7-year-old male patient who was born at 39 weeks gestation to gravida 3 para 3 following induced labor due to elevated maternal blood pressure. During the first 2 years of life, his growth and development were normal and his immunizations were up to date. The patient's medical history included upper respiratory tract infections (URIs), respiratory syncytial virus, as well as 3 bouts of pneumonia and multiple otitis media that resulted in 18 rounds of antibiotics. The child was also allergic to nuts and milk protein. The patient’s parents are of Northern European and Native American descent. There is no known family history of eye, ear, or kidney diseases.
Renal concerns were first noted at the age of 2 years and 6 months when he presented to an emergency department in Fall 2019 (week 0) for several weeks of intermittent dark-colored urine. His mother reported that the discoloration recently progressed in intensity to cola-colored, along with the onset of persistent vomiting without any fever or diarrhea. On physical examination, the patient had normal vitals: weight 14.8 kg (68th percentile), height 91 cm (24th percentile), and body surface area 0.6 m2. There was no edema, rash, or lymphadenopathy, but he appeared pale.
The patient’s initial laboratory results included: complete blood count with white blood cells (WBC) 10 x 103/L (reference range, 4.5-13.5 x 103/L); differential lymphocytes 69%; neutrophils 21%; hemoglobin 10 g/dL (reference range, 12-16 g/dL); hematocrit, 30%; (reference range, 37%-45%); platelets 437 103/L (reference range, 150-450 x 103/L); serum creatinine 0.46 mg/dL (reference range, 0.5-0.9 mg/dL); and albumin 3.1 g/dL (reference range, 3.5-5.2 g/dL). Serum electrolyte levels and liver enzymes were normal. A urine analysis revealed 3+ protein and 3+ blood with dysmorphic red blood cells (RBC) and RBC casts without WBC. The patient's spot urine protein-to-creatinine ratio was 4.3 and his renal ultrasound was normal. The patient was referred to Nephrology.
During the next 2 weeks, his protein-to-creatinine ratio progressed to 5.9 and serum albumin fell to 2.7 g/dL. His urine remained red colored, and a microscopic examination with RBC > 500 and WBC up to 10 on a high powered field. His workup was negative for antinuclear antibodies, antineutrophil cytoplasmic antibody, antistreptolysin-O (ASO) and anti-DNase B. Serum C3 was low at 81 mg/dL (reference range, 90-180 mg/dL), C4 was 13.3 mg/dL (reference range, 10-40 mg/dL), and immunoglobulin G was low at 452 mg/dL (reference range 719-1475 mg/dL). A baseline audiology test revealed normal hearing.
Percutaneous renal biopsy yielded about 12 glomeruli, all exhibiting mild mesangial matrix expansion and hypercellularity (Figure 1). One glomerulus had prominent parietal epithelial cells without endocapillary hypercellularity or crescent formation. There was no interstitial fibrosis or tubular atrophy. Immunofluorescence studies showed no evidence of immune complex deposition with negative staining for immunoglobulin heavy and light chains, C3 and C1q. Staining for α 2 and α 5 units of collagen was normal. Electron microscopy showed patchy areas of severe basement membrane thinning with frequent foci of mild to moderate lamina densa splitting and associated visceral epithelial cell foot process effacement (Figure 2).
These were reported as concerning findings for possible Alport syndrome by 3 independent pathology teams. The genetic testing was submitted at a commercial laboratory to screen 17 mutations, including COL4A3, COL4A4, and COL4A5. Results showed the presence of a heterozygous VUS in the COL4A4 gene (c.1055C > T; p.Pro352Leu; dbSNP ID: rs371717486; PolyPhen-2: Probably Damaging; SIFT: Deleterious) as well as the presence of a heterozygous VUS in TRPC6 gene (c2463A>T; p.Lys821Asn; dbSNP ID: rs199948731; PolyPhen-2: Benign; SIFT: Tolerated). Further genetic investigation by whole exome sequencing on approximately 20,000 genes through MNG Laboratories showed a new heterozygous VUS in the OSGEP gene [c.328T>C; p.Cys110Arg]. Additional studies ruled out mitochondrial disease, CoQ10 deficiency, and metabolic disorders upon normal findings for mitochondrial DNA, urine amino acids, plasma acylcarnitine profile, orotic acid, ammonia, and homocysteine levels.
Figure 3 summarizes the patient’s treatment response during 170 weeks of follow-up (Fall 2019 to Summer 2023). The patient was started on enalapril 0.6 mg/kg daily at week 3, which continued throughout treatment. Following a rheumatology consult at week 30, the patient was started on prednisolone 3 mg/mL to assess the role of inflammation through the treatment response. An initial dose of 2 mg/kg daily (9 mL) for 1 month was followed by every other day treatment that was tapered off by week 48. To control mild but noticeably increasing proteinuria in the interim, subcutaneous anakinra 50 mg (3 mg/kg daily) was added as a steroid
DISCUSSION
This case describes a child with rapidly progressive proteinuria and hematuria following a URI who was found to have VUS mutations in 3 different genes associated with chronic kidney disease. Serology tests on the patient were negative for streptococcal antibodies and antinuclear antibodies, ruling out poststreptococcal glomerulonephritis, or systemic lupus erythematosus. His renal biopsy findings were concerning for altered podocytes, mesangial cells, and basement membrane without inflammatory infiltrate, immune complex, complements, immunoglobulin A, or vasculopathy. His blood inflammatory markers, erythrocyte sedimentation rate, C-reactive protein, and ferritin were normal when his care team initiated daily steroids.
Overall, the patient’s clinical presentation and histopathology findings were suggestive of Alport syndrome or thin basement membrane nephropathy with a high potential to progress into FSGS.10-12 Alport syndrome affects 1 in 5000 to 10,000 children annually due to S-linked inheritance of COL4A5, or autosomal recessive inheritance of COL4A3 or COL4A4 genes. It presents with hematuria and hearing loss.10 Our patient had a single copy COL4A4 gene mutation that was classified as VUS. He also had 2 additional VUS affecting the TRPC6 and OSGEP genes. TRPC6 gene mutation can be associated with FSGS through autosomal dominant inheritance. Both COL4A4 and TRPC6 gene mutations were paternally inherited. Although the patient’s father not having renal disease argues against the clinical significance of these findings, there is literature on the potential role of heterozygous COL4A4 variant mimicking thin basement membrane nephropathy that can lead to renal impairment upon copresence of superimposed conditions.13 The patient’s rapidly progressing hematuria and changes in the basement membrane were worrisome for emerging FSGS. Furthermore, VUS of TRPC6 has been reported in late onset autosomal dominant FSGS and can be associated with early onset steroid-resistant nephrotic syndrome (NS) in children.14 This concern was voiced by 3 nephrology consultants during the initial evaluation, leading to the consensus that steroid treatment for podocytopathy would not alter the patient’s long-term outcomes (ie, progression to FSGS).
Immunomodulation
Our rationale for immunomodulatory treatment was based on the abrupt onset of renal concerns following a URI, suggesting the importance of an inflammatory trigger causing altered homeostasis in a genetically susceptible host. Preclinical models show that microbial products such as lipopolysaccharides can lead to podocytopathy by several mechanisms through activation of toll-like receptor signaling. It can directly cause apoptosis by downregulation of the intracellular Akt survival pathway.15 Lipopolysaccharide can also activate the NF-αB pathway and upregulate the production of interleukin-1 (IL-1) and TNF-α in mesangial cells.16,17
Both cytokines can promote mesangial cell proliferation.18 Through autocrine and paracrine mechanisms, proinflammatory cytokines can further perpetuate somatic tissue changes and contribute to the development of podocytopathy. For instance, TNF-α can promote podocyte injury and proteinuria by downregulation of the slit diaphragm protein expression (ie, nephrin, ezrin, or podocin), and disruption of podocyte cytoskeleton.19,20 TNF-α promotes the influx and activation of macrophages and inflammatory cells. It is actively involved in chronic alterations within the glomeruli by the upregulation of matrix metalloproteases by integrins, as well as activation of myofibroblast progenitors and extracellular matrix deposition in crosstalk with transforming growth factor and other key mediators.17,21,22
For the patient described in this case report, initial improvement on steroids encouraged the pursuit of additional treatment to downregulate inflammatory pathways within the glomerular milieu. However, within the COVID-19 environment, escalating the patient’s treatment using traditional immunomodulators (ie, calcineurin inhibitors or mycophenolate mofetil) was not favored due to the risk of infection. Initially, anakinra, a recombinant IL-1 receptor antagonist, was preferred as a steroid-sparing agent for its short life and safety profile during the pandemic. At first, the patient responded well to anakinra and was allowed a steroid wean when the dose was titrated up to 6 mg/kg daily. However, anakinra did not prevent the escalation of proteinuria following a URI. After the treatment was changed to adalimumab, a fully humanized monoclonal antibody to TNF-α, the patient continued to improve and reach full remission despite experiencing a cold and the flu in the following months.
Literature Review
There is a paucity of literature on applications of biological response modifiers for idiopathic NS and FSGS.23,24 Angeletti and colleagues reported that 3 patients with severe long-standing FSGS benefited from anakinra 4 mg/kg daily to reduce proteinuria and improve kidney function. All the patients had positive C3 staining in renal biopsy and treatment response, which supported the role of C3a in inducing podocyte injury through upregulated expression of IL-1 and IL-1R.23 Trachtman and colleagues reported on the phase II FONT trial that included 14 of 21 patients aged < 18 years with advanced FSGS who were treated with adalimumab 24 mg/m2, or ≤ 40 mg every other week.24 Although, during a 6-month period, none of the 7 patients met the endpoint of reduced proteinuria by ≥ 50%, and the authors suggested that careful patient selection may improve the treatment response in future trials.24
A recent study involving transcriptomics on renal tissue samples combined with available pathology (fibrosis), urinary markers, and clinical characteristics on 285 patients with MCD or FSGS from 3 different continents identified 3 distinct clusters. Patients with evidence of activated kidney TNF pathway (n = 72, aged > 18 years) were found to have poor clinical outcomes.25 The study identified 2 urine markers associated with the TNF pathway (ie, tissue inhibitor of metalloproteinases-1 and monocyte chemoattractant protein-1), which aligns with the preclinical findings previously mentioned.25
Conclusions
The patient’s condition in this case illustrates the complex nature of biologically predetermined cascading events in the emergence of glomerular disease upon environmental triggers under the influence of genetic factors.
Chronic kidney disease affects 7.7% of veterans annually, illustrating the need for new therapeutics.26 Based on our experience and literature review, upregulation of TNF-α is a root cause of glomerulopathy; further studies are warranted to evaluate the efficacy of anti-TNF biologic response modifiers for the treatment of these patients. Long-term postmarketing safety profile and steroid-sparing properties of adalimumab should allow inclusion of pediatric cases in future trials. Results may also contribute to identifying new predictive biomarkers related to the basement membrane when combined with precision nephrology to further advance patient selection and targeted treatment.25,27
Acknowledgments
The authors thank the patient’s mother for providing consent to allow publication of this case report.
1. Arif E, Nihalani D. Glomerular filtration barrier assembly: an insight. Postdoc J. 2013;1(4):33-45.
2. Garg PA. Review of podocyte biology. Am J Nephrol. 2018;47(suppl 1):3-13. doi:10.1159/000481633SUPPL
3. Warady BA, Agarwal R, Bangalore S, et al. Alport syndrome classification and management. Kidney Med. 2020;2(5):639-649. doi:10.1016/j.xkme.2020.05.014
4. Angioi A, Pani A. FSGS: from pathogenesis to the histological lesion. J Nephrol. 2016;29(4):517-523. doi:10.1007/s40620-016-0333-2
5. Roca N, Martinez C, Jatem E, Madrid A, Lopez M, Segarra A. Activation of the acute inflammatory phase response in idiopathic nephrotic syndrome: association with clinicopathological phenotypes and with response to corticosteroids. Clin Kidney J. 2021;14(4):1207-1215. doi:10.1093/ckj/sfaa247
6. Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal change disease. Clin J Am Soc Nephrol. 2017;12(2):332-345.
7. Medjeral-Thomas NR, Lawrence C, Condon M, et al. Randomized, controlled trial of tacrolimus and prednisolone monotherapy for adults with De Novo minimal change disease: a multicenter, randomized, controlled trial. Clin J Am Soc Nephrol. 2020;15(2):209-218. doi:10.2215/CJN.06290420
8. Ye Q, Lan B, Liu H, Persson PB, Lai EY, Mao J. A critical role of the podocyte cytoskeleton in the pathogenesis of glomerular proteinuria and autoimmune podocytopathies. Acta Physiol (Oxf). 2022;235(4):e13850. doi:10.1111/apha.13850
9. Trautmann A, Schnaidt S, Lipska-Ziμtkiewicz BS, et al. Long-term outcome of steroid-resistant nephrotic syndrome in children. J Am Soc Nephrol. 2017;28:3055-3065. doi:10.1681/ASN.2016101121
10. Kashtan CE, Gross O. Clinical practice recommendations for the diagnosis and management of Alport syndrome in children, adolescents, and young adults-an update for 2020. Pediatr Nephrol. 2021;36(3):711-719. doi:10.1007/s00467-020-04819-6
11. Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY. Thin basement membrane nephropathy. Kidney Int. 2003;64(4):1169-78. doi:10.1046/j.1523-1755.2003.00234.x
12. Rosenberg AZ, Kopp JB. Focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2017; 12(3):502-517. doi:10.2215/CJN.05960616
13. Savige J. Should we diagnose autosomal dominant Alport syndrome when there is a pathogenic heterozygous COL4A3 or COL4A4 variant? Kidney Int Rep. 2018;3(6):1239-1241. doi:10.1016/j.ekir.2018.08.002
14. Gigante M, Caridi G, Montemurno E, et al. TRPC6 mutations in children with steroid-resistant nephrotic syndrome and atypical phenotype. Clin J Am Soc Nephrol. 2011;6(7):1626-1634. doi:10.2215/CJN.07830910
15. Saurus P, Kuusela S, Lehtonen E, et al. Podocyte apoptosis is prevented by blocking the toll-like receptor pathway. Cell Death Dis. 2015;6(5):e1752. doi:10.1038/cddis.2015.125
16. Baud L, Oudinet JP, Bens M, et al. Production of tumor necrosis factor by rat mesangial cells in response to bacterial lipopolysaccharide. Kidney Int. 1989;35(5):1111-1118. doi:10.1038/ki.1989.98
17. White S, Lin L, Hu K. NF-κB and tPA signaling in kidney and other diseases. Cells. 2020;9(6):1348. doi:10.3390/cells9061348
18. Tesch GH, Lan HY, Atkins RC, Nikolic-Paterson DJ. Role of interleukin-1 in mesangial cell proliferation and matrix deposition in experimental mesangioproliferative nephritis. Am J Pathol. 1997;151(1):141-150.
19. Lai KN, Leung JCK, Chan LYY, et al. Podocyte injury induced by mesangial-derived cytokines in IgA Nephropathy. Nephrol Dial Transplant. 2009;24(1):62-72. doi:10.1093/ndt/gfn441
20. Saleem MA, Kobayashi Y. Cell biology and genetics of minimal change disease. F1000 Res. 2016;5: F1000 Faculty Rev-412. doi:10.12688/f1000research.7300.1
21. Kim KP, Williams CE, Lemmon CA. Cell-matrix interactions in renal fibrosis. Kidney Dial. 2022;2(4):607-624. doi:10.3390/kidneydial2040055
22. Zvaifler NJ. Relevance of the stroma and epithelial-mesenchymal transition (EMT) for the rheumatic diseases. Arthritis Res Ther. 2006;8(3):210. doi:10.1186/ar1963
23. Angeletti A, Magnasco A, Trivelli A, et al. Refractory minimal change disease and focal segmental glomerular sclerosis treated with Anakinra. Kidney Int Rep. 2021;7(1):121-124. doi:10.1016/j.ekir.2021.10.018
24. Trachtman H, Vento S, Herreshoff E, et al. Efficacy of galactose and adalimumab in patients with resistant focal segmental glomerulosclerosis: report of the font clinical trial group. BMC Nephrol. 2015;16:111. doi:10.1186/s12882-015-0094-5
25. Mariani LH, Eddy S, AlAkwaa FM, et al. Precision nephrology identified tumor necrosis factor activation variability in minimal change disease and focal segmental glomerulosclerosis. Kidney Int. 2023;103(3):565-579. doi:10.1016/j.kint.2022.10.023
26. Korshak L, Washington DL, Powell J, Nylen E, Kokkinos P. Kidney Disease in Veterans. US Dept of Veterans Affairs, Office of Health Equity. Updated May 13, 2020. Accessed June 28, 2024. https://www.va.gov/HEALTHEQUITY/Kidney_Disease_In_Veterans.asp
27. Malone AF, Phelan PJ, Hall G, et al. Rare hereditary COL4A3/COL4A4 variants may be mistaken for familial focal segmental glomerulosclerosis. Kidney Int. 2014;86(6):1253-1259. doi:10.1038/ki.2014.305
Podocytes are terminally differentiated, highly specialized cells located in juxtaposition to the basement membrane over the abluminal surfaces of endothelial cells within the glomerular tuft. This triad structure is the site of the filtration barrier, which forms highly delicate and tightly regulated architecture to carry out the ultrafiltration function of the kidney.1 The filtration barrier is characterized by foot processes that are connected by specialized junctions called slit diaphragms.
Insults to components of the filtration barrier can initiate cascading events and perpetuate structural alterations that may eventually result in sclerotic changes.2 Common causes among children include minimal change disease (MCD) with the collapse of foot processes resulting in proteinuria, Alport syndrome due to mutation of collagen fibers within the basement membrane leading to hematuria and proteinuria, immune complex mediated nephropathy following common infections or autoimmune diseases, and focal segmental glomerulosclerosis (FSGS) that can show variable histopathology toward eventual glomerular scarring.3,4 These children often clinically have minimal, if any, signs of systemic inflammation.3-5 This has been a limiting factor for the commitment to immunomodulatory treatment, except for steroids for the treatment of MCD.6 Although prolonged steroid treatment may be efficacious, adverse effects are significant in a growing child. Alternative treatments, such as tacrolimus and rituximab have been suggested as second-line steroid-sparing agents.7,8 Not uncommonly, however, these cases are managed by supportive measures only during the progression of the natural course of the disease, which may eventually lead to renal failure, requiring transplant for survival.8,9
This case report highlights a child with a variant of uncertain significance (VUS) in genes involved in Alport syndrome and FSGS who developed an abrupt onset of proteinuria and hematuria after a respiratory illness. To our knowledge, he represents the youngest case demonstrating the benefit of targeted treatment against tumor necrosis factor-α (TNF-α) for glomerulopathy using biologic response modifiers.
Case Description
This is currently a 7-year-old male patient who was born at 39 weeks gestation to gravida 3 para 3 following induced labor due to elevated maternal blood pressure. During the first 2 years of life, his growth and development were normal and his immunizations were up to date. The patient's medical history included upper respiratory tract infections (URIs), respiratory syncytial virus, as well as 3 bouts of pneumonia and multiple otitis media that resulted in 18 rounds of antibiotics. The child was also allergic to nuts and milk protein. The patient’s parents are of Northern European and Native American descent. There is no known family history of eye, ear, or kidney diseases.
Renal concerns were first noted at the age of 2 years and 6 months when he presented to an emergency department in Fall 2019 (week 0) for several weeks of intermittent dark-colored urine. His mother reported that the discoloration recently progressed in intensity to cola-colored, along with the onset of persistent vomiting without any fever or diarrhea. On physical examination, the patient had normal vitals: weight 14.8 kg (68th percentile), height 91 cm (24th percentile), and body surface area 0.6 m2. There was no edema, rash, or lymphadenopathy, but he appeared pale.
The patient’s initial laboratory results included: complete blood count with white blood cells (WBC) 10 x 103/L (reference range, 4.5-13.5 x 103/L); differential lymphocytes 69%; neutrophils 21%; hemoglobin 10 g/dL (reference range, 12-16 g/dL); hematocrit, 30%; (reference range, 37%-45%); platelets 437 103/L (reference range, 150-450 x 103/L); serum creatinine 0.46 mg/dL (reference range, 0.5-0.9 mg/dL); and albumin 3.1 g/dL (reference range, 3.5-5.2 g/dL). Serum electrolyte levels and liver enzymes were normal. A urine analysis revealed 3+ protein and 3+ blood with dysmorphic red blood cells (RBC) and RBC casts without WBC. The patient's spot urine protein-to-creatinine ratio was 4.3 and his renal ultrasound was normal. The patient was referred to Nephrology.
During the next 2 weeks, his protein-to-creatinine ratio progressed to 5.9 and serum albumin fell to 2.7 g/dL. His urine remained red colored, and a microscopic examination with RBC > 500 and WBC up to 10 on a high powered field. His workup was negative for antinuclear antibodies, antineutrophil cytoplasmic antibody, antistreptolysin-O (ASO) and anti-DNase B. Serum C3 was low at 81 mg/dL (reference range, 90-180 mg/dL), C4 was 13.3 mg/dL (reference range, 10-40 mg/dL), and immunoglobulin G was low at 452 mg/dL (reference range 719-1475 mg/dL). A baseline audiology test revealed normal hearing.
Percutaneous renal biopsy yielded about 12 glomeruli, all exhibiting mild mesangial matrix expansion and hypercellularity (Figure 1). One glomerulus had prominent parietal epithelial cells without endocapillary hypercellularity or crescent formation. There was no interstitial fibrosis or tubular atrophy. Immunofluorescence studies showed no evidence of immune complex deposition with negative staining for immunoglobulin heavy and light chains, C3 and C1q. Staining for α 2 and α 5 units of collagen was normal. Electron microscopy showed patchy areas of severe basement membrane thinning with frequent foci of mild to moderate lamina densa splitting and associated visceral epithelial cell foot process effacement (Figure 2).
These were reported as concerning findings for possible Alport syndrome by 3 independent pathology teams. The genetic testing was submitted at a commercial laboratory to screen 17 mutations, including COL4A3, COL4A4, and COL4A5. Results showed the presence of a heterozygous VUS in the COL4A4 gene (c.1055C > T; p.Pro352Leu; dbSNP ID: rs371717486; PolyPhen-2: Probably Damaging; SIFT: Deleterious) as well as the presence of a heterozygous VUS in TRPC6 gene (c2463A>T; p.Lys821Asn; dbSNP ID: rs199948731; PolyPhen-2: Benign; SIFT: Tolerated). Further genetic investigation by whole exome sequencing on approximately 20,000 genes through MNG Laboratories showed a new heterozygous VUS in the OSGEP gene [c.328T>C; p.Cys110Arg]. Additional studies ruled out mitochondrial disease, CoQ10 deficiency, and metabolic disorders upon normal findings for mitochondrial DNA, urine amino acids, plasma acylcarnitine profile, orotic acid, ammonia, and homocysteine levels.
Figure 3 summarizes the patient’s treatment response during 170 weeks of follow-up (Fall 2019 to Summer 2023). The patient was started on enalapril 0.6 mg/kg daily at week 3, which continued throughout treatment. Following a rheumatology consult at week 30, the patient was started on prednisolone 3 mg/mL to assess the role of inflammation through the treatment response. An initial dose of 2 mg/kg daily (9 mL) for 1 month was followed by every other day treatment that was tapered off by week 48. To control mild but noticeably increasing proteinuria in the interim, subcutaneous anakinra 50 mg (3 mg/kg daily) was added as a steroid
DISCUSSION
This case describes a child with rapidly progressive proteinuria and hematuria following a URI who was found to have VUS mutations in 3 different genes associated with chronic kidney disease. Serology tests on the patient were negative for streptococcal antibodies and antinuclear antibodies, ruling out poststreptococcal glomerulonephritis, or systemic lupus erythematosus. His renal biopsy findings were concerning for altered podocytes, mesangial cells, and basement membrane without inflammatory infiltrate, immune complex, complements, immunoglobulin A, or vasculopathy. His blood inflammatory markers, erythrocyte sedimentation rate, C-reactive protein, and ferritin were normal when his care team initiated daily steroids.
Overall, the patient’s clinical presentation and histopathology findings were suggestive of Alport syndrome or thin basement membrane nephropathy with a high potential to progress into FSGS.10-12 Alport syndrome affects 1 in 5000 to 10,000 children annually due to S-linked inheritance of COL4A5, or autosomal recessive inheritance of COL4A3 or COL4A4 genes. It presents with hematuria and hearing loss.10 Our patient had a single copy COL4A4 gene mutation that was classified as VUS. He also had 2 additional VUS affecting the TRPC6 and OSGEP genes. TRPC6 gene mutation can be associated with FSGS through autosomal dominant inheritance. Both COL4A4 and TRPC6 gene mutations were paternally inherited. Although the patient’s father not having renal disease argues against the clinical significance of these findings, there is literature on the potential role of heterozygous COL4A4 variant mimicking thin basement membrane nephropathy that can lead to renal impairment upon copresence of superimposed conditions.13 The patient’s rapidly progressing hematuria and changes in the basement membrane were worrisome for emerging FSGS. Furthermore, VUS of TRPC6 has been reported in late onset autosomal dominant FSGS and can be associated with early onset steroid-resistant nephrotic syndrome (NS) in children.14 This concern was voiced by 3 nephrology consultants during the initial evaluation, leading to the consensus that steroid treatment for podocytopathy would not alter the patient’s long-term outcomes (ie, progression to FSGS).
Immunomodulation
Our rationale for immunomodulatory treatment was based on the abrupt onset of renal concerns following a URI, suggesting the importance of an inflammatory trigger causing altered homeostasis in a genetically susceptible host. Preclinical models show that microbial products such as lipopolysaccharides can lead to podocytopathy by several mechanisms through activation of toll-like receptor signaling. It can directly cause apoptosis by downregulation of the intracellular Akt survival pathway.15 Lipopolysaccharide can also activate the NF-αB pathway and upregulate the production of interleukin-1 (IL-1) and TNF-α in mesangial cells.16,17
Both cytokines can promote mesangial cell proliferation.18 Through autocrine and paracrine mechanisms, proinflammatory cytokines can further perpetuate somatic tissue changes and contribute to the development of podocytopathy. For instance, TNF-α can promote podocyte injury and proteinuria by downregulation of the slit diaphragm protein expression (ie, nephrin, ezrin, or podocin), and disruption of podocyte cytoskeleton.19,20 TNF-α promotes the influx and activation of macrophages and inflammatory cells. It is actively involved in chronic alterations within the glomeruli by the upregulation of matrix metalloproteases by integrins, as well as activation of myofibroblast progenitors and extracellular matrix deposition in crosstalk with transforming growth factor and other key mediators.17,21,22
For the patient described in this case report, initial improvement on steroids encouraged the pursuit of additional treatment to downregulate inflammatory pathways within the glomerular milieu. However, within the COVID-19 environment, escalating the patient’s treatment using traditional immunomodulators (ie, calcineurin inhibitors or mycophenolate mofetil) was not favored due to the risk of infection. Initially, anakinra, a recombinant IL-1 receptor antagonist, was preferred as a steroid-sparing agent for its short life and safety profile during the pandemic. At first, the patient responded well to anakinra and was allowed a steroid wean when the dose was titrated up to 6 mg/kg daily. However, anakinra did not prevent the escalation of proteinuria following a URI. After the treatment was changed to adalimumab, a fully humanized monoclonal antibody to TNF-α, the patient continued to improve and reach full remission despite experiencing a cold and the flu in the following months.
Literature Review
There is a paucity of literature on applications of biological response modifiers for idiopathic NS and FSGS.23,24 Angeletti and colleagues reported that 3 patients with severe long-standing FSGS benefited from anakinra 4 mg/kg daily to reduce proteinuria and improve kidney function. All the patients had positive C3 staining in renal biopsy and treatment response, which supported the role of C3a in inducing podocyte injury through upregulated expression of IL-1 and IL-1R.23 Trachtman and colleagues reported on the phase II FONT trial that included 14 of 21 patients aged < 18 years with advanced FSGS who were treated with adalimumab 24 mg/m2, or ≤ 40 mg every other week.24 Although, during a 6-month period, none of the 7 patients met the endpoint of reduced proteinuria by ≥ 50%, and the authors suggested that careful patient selection may improve the treatment response in future trials.24
A recent study involving transcriptomics on renal tissue samples combined with available pathology (fibrosis), urinary markers, and clinical characteristics on 285 patients with MCD or FSGS from 3 different continents identified 3 distinct clusters. Patients with evidence of activated kidney TNF pathway (n = 72, aged > 18 years) were found to have poor clinical outcomes.25 The study identified 2 urine markers associated with the TNF pathway (ie, tissue inhibitor of metalloproteinases-1 and monocyte chemoattractant protein-1), which aligns with the preclinical findings previously mentioned.25
Conclusions
The patient’s condition in this case illustrates the complex nature of biologically predetermined cascading events in the emergence of glomerular disease upon environmental triggers under the influence of genetic factors.
Chronic kidney disease affects 7.7% of veterans annually, illustrating the need for new therapeutics.26 Based on our experience and literature review, upregulation of TNF-α is a root cause of glomerulopathy; further studies are warranted to evaluate the efficacy of anti-TNF biologic response modifiers for the treatment of these patients. Long-term postmarketing safety profile and steroid-sparing properties of adalimumab should allow inclusion of pediatric cases in future trials. Results may also contribute to identifying new predictive biomarkers related to the basement membrane when combined with precision nephrology to further advance patient selection and targeted treatment.25,27
Acknowledgments
The authors thank the patient’s mother for providing consent to allow publication of this case report.
Podocytes are terminally differentiated, highly specialized cells located in juxtaposition to the basement membrane over the abluminal surfaces of endothelial cells within the glomerular tuft. This triad structure is the site of the filtration barrier, which forms highly delicate and tightly regulated architecture to carry out the ultrafiltration function of the kidney.1 The filtration barrier is characterized by foot processes that are connected by specialized junctions called slit diaphragms.
Insults to components of the filtration barrier can initiate cascading events and perpetuate structural alterations that may eventually result in sclerotic changes.2 Common causes among children include minimal change disease (MCD) with the collapse of foot processes resulting in proteinuria, Alport syndrome due to mutation of collagen fibers within the basement membrane leading to hematuria and proteinuria, immune complex mediated nephropathy following common infections or autoimmune diseases, and focal segmental glomerulosclerosis (FSGS) that can show variable histopathology toward eventual glomerular scarring.3,4 These children often clinically have minimal, if any, signs of systemic inflammation.3-5 This has been a limiting factor for the commitment to immunomodulatory treatment, except for steroids for the treatment of MCD.6 Although prolonged steroid treatment may be efficacious, adverse effects are significant in a growing child. Alternative treatments, such as tacrolimus and rituximab have been suggested as second-line steroid-sparing agents.7,8 Not uncommonly, however, these cases are managed by supportive measures only during the progression of the natural course of the disease, which may eventually lead to renal failure, requiring transplant for survival.8,9
This case report highlights a child with a variant of uncertain significance (VUS) in genes involved in Alport syndrome and FSGS who developed an abrupt onset of proteinuria and hematuria after a respiratory illness. To our knowledge, he represents the youngest case demonstrating the benefit of targeted treatment against tumor necrosis factor-α (TNF-α) for glomerulopathy using biologic response modifiers.
Case Description
This is currently a 7-year-old male patient who was born at 39 weeks gestation to gravida 3 para 3 following induced labor due to elevated maternal blood pressure. During the first 2 years of life, his growth and development were normal and his immunizations were up to date. The patient's medical history included upper respiratory tract infections (URIs), respiratory syncytial virus, as well as 3 bouts of pneumonia and multiple otitis media that resulted in 18 rounds of antibiotics. The child was also allergic to nuts and milk protein. The patient’s parents are of Northern European and Native American descent. There is no known family history of eye, ear, or kidney diseases.
Renal concerns were first noted at the age of 2 years and 6 months when he presented to an emergency department in Fall 2019 (week 0) for several weeks of intermittent dark-colored urine. His mother reported that the discoloration recently progressed in intensity to cola-colored, along with the onset of persistent vomiting without any fever or diarrhea. On physical examination, the patient had normal vitals: weight 14.8 kg (68th percentile), height 91 cm (24th percentile), and body surface area 0.6 m2. There was no edema, rash, or lymphadenopathy, but he appeared pale.
The patient’s initial laboratory results included: complete blood count with white blood cells (WBC) 10 x 103/L (reference range, 4.5-13.5 x 103/L); differential lymphocytes 69%; neutrophils 21%; hemoglobin 10 g/dL (reference range, 12-16 g/dL); hematocrit, 30%; (reference range, 37%-45%); platelets 437 103/L (reference range, 150-450 x 103/L); serum creatinine 0.46 mg/dL (reference range, 0.5-0.9 mg/dL); and albumin 3.1 g/dL (reference range, 3.5-5.2 g/dL). Serum electrolyte levels and liver enzymes were normal. A urine analysis revealed 3+ protein and 3+ blood with dysmorphic red blood cells (RBC) and RBC casts without WBC. The patient's spot urine protein-to-creatinine ratio was 4.3 and his renal ultrasound was normal. The patient was referred to Nephrology.
During the next 2 weeks, his protein-to-creatinine ratio progressed to 5.9 and serum albumin fell to 2.7 g/dL. His urine remained red colored, and a microscopic examination with RBC > 500 and WBC up to 10 on a high powered field. His workup was negative for antinuclear antibodies, antineutrophil cytoplasmic antibody, antistreptolysin-O (ASO) and anti-DNase B. Serum C3 was low at 81 mg/dL (reference range, 90-180 mg/dL), C4 was 13.3 mg/dL (reference range, 10-40 mg/dL), and immunoglobulin G was low at 452 mg/dL (reference range 719-1475 mg/dL). A baseline audiology test revealed normal hearing.
Percutaneous renal biopsy yielded about 12 glomeruli, all exhibiting mild mesangial matrix expansion and hypercellularity (Figure 1). One glomerulus had prominent parietal epithelial cells without endocapillary hypercellularity or crescent formation. There was no interstitial fibrosis or tubular atrophy. Immunofluorescence studies showed no evidence of immune complex deposition with negative staining for immunoglobulin heavy and light chains, C3 and C1q. Staining for α 2 and α 5 units of collagen was normal. Electron microscopy showed patchy areas of severe basement membrane thinning with frequent foci of mild to moderate lamina densa splitting and associated visceral epithelial cell foot process effacement (Figure 2).
These were reported as concerning findings for possible Alport syndrome by 3 independent pathology teams. The genetic testing was submitted at a commercial laboratory to screen 17 mutations, including COL4A3, COL4A4, and COL4A5. Results showed the presence of a heterozygous VUS in the COL4A4 gene (c.1055C > T; p.Pro352Leu; dbSNP ID: rs371717486; PolyPhen-2: Probably Damaging; SIFT: Deleterious) as well as the presence of a heterozygous VUS in TRPC6 gene (c2463A>T; p.Lys821Asn; dbSNP ID: rs199948731; PolyPhen-2: Benign; SIFT: Tolerated). Further genetic investigation by whole exome sequencing on approximately 20,000 genes through MNG Laboratories showed a new heterozygous VUS in the OSGEP gene [c.328T>C; p.Cys110Arg]. Additional studies ruled out mitochondrial disease, CoQ10 deficiency, and metabolic disorders upon normal findings for mitochondrial DNA, urine amino acids, plasma acylcarnitine profile, orotic acid, ammonia, and homocysteine levels.
Figure 3 summarizes the patient’s treatment response during 170 weeks of follow-up (Fall 2019 to Summer 2023). The patient was started on enalapril 0.6 mg/kg daily at week 3, which continued throughout treatment. Following a rheumatology consult at week 30, the patient was started on prednisolone 3 mg/mL to assess the role of inflammation through the treatment response. An initial dose of 2 mg/kg daily (9 mL) for 1 month was followed by every other day treatment that was tapered off by week 48. To control mild but noticeably increasing proteinuria in the interim, subcutaneous anakinra 50 mg (3 mg/kg daily) was added as a steroid
DISCUSSION
This case describes a child with rapidly progressive proteinuria and hematuria following a URI who was found to have VUS mutations in 3 different genes associated with chronic kidney disease. Serology tests on the patient were negative for streptococcal antibodies and antinuclear antibodies, ruling out poststreptococcal glomerulonephritis, or systemic lupus erythematosus. His renal biopsy findings were concerning for altered podocytes, mesangial cells, and basement membrane without inflammatory infiltrate, immune complex, complements, immunoglobulin A, or vasculopathy. His blood inflammatory markers, erythrocyte sedimentation rate, C-reactive protein, and ferritin were normal when his care team initiated daily steroids.
Overall, the patient’s clinical presentation and histopathology findings were suggestive of Alport syndrome or thin basement membrane nephropathy with a high potential to progress into FSGS.10-12 Alport syndrome affects 1 in 5000 to 10,000 children annually due to S-linked inheritance of COL4A5, or autosomal recessive inheritance of COL4A3 or COL4A4 genes. It presents with hematuria and hearing loss.10 Our patient had a single copy COL4A4 gene mutation that was classified as VUS. He also had 2 additional VUS affecting the TRPC6 and OSGEP genes. TRPC6 gene mutation can be associated with FSGS through autosomal dominant inheritance. Both COL4A4 and TRPC6 gene mutations were paternally inherited. Although the patient’s father not having renal disease argues against the clinical significance of these findings, there is literature on the potential role of heterozygous COL4A4 variant mimicking thin basement membrane nephropathy that can lead to renal impairment upon copresence of superimposed conditions.13 The patient’s rapidly progressing hematuria and changes in the basement membrane were worrisome for emerging FSGS. Furthermore, VUS of TRPC6 has been reported in late onset autosomal dominant FSGS and can be associated with early onset steroid-resistant nephrotic syndrome (NS) in children.14 This concern was voiced by 3 nephrology consultants during the initial evaluation, leading to the consensus that steroid treatment for podocytopathy would not alter the patient’s long-term outcomes (ie, progression to FSGS).
Immunomodulation
Our rationale for immunomodulatory treatment was based on the abrupt onset of renal concerns following a URI, suggesting the importance of an inflammatory trigger causing altered homeostasis in a genetically susceptible host. Preclinical models show that microbial products such as lipopolysaccharides can lead to podocytopathy by several mechanisms through activation of toll-like receptor signaling. It can directly cause apoptosis by downregulation of the intracellular Akt survival pathway.15 Lipopolysaccharide can also activate the NF-αB pathway and upregulate the production of interleukin-1 (IL-1) and TNF-α in mesangial cells.16,17
Both cytokines can promote mesangial cell proliferation.18 Through autocrine and paracrine mechanisms, proinflammatory cytokines can further perpetuate somatic tissue changes and contribute to the development of podocytopathy. For instance, TNF-α can promote podocyte injury and proteinuria by downregulation of the slit diaphragm protein expression (ie, nephrin, ezrin, or podocin), and disruption of podocyte cytoskeleton.19,20 TNF-α promotes the influx and activation of macrophages and inflammatory cells. It is actively involved in chronic alterations within the glomeruli by the upregulation of matrix metalloproteases by integrins, as well as activation of myofibroblast progenitors and extracellular matrix deposition in crosstalk with transforming growth factor and other key mediators.17,21,22
For the patient described in this case report, initial improvement on steroids encouraged the pursuit of additional treatment to downregulate inflammatory pathways within the glomerular milieu. However, within the COVID-19 environment, escalating the patient’s treatment using traditional immunomodulators (ie, calcineurin inhibitors or mycophenolate mofetil) was not favored due to the risk of infection. Initially, anakinra, a recombinant IL-1 receptor antagonist, was preferred as a steroid-sparing agent for its short life and safety profile during the pandemic. At first, the patient responded well to anakinra and was allowed a steroid wean when the dose was titrated up to 6 mg/kg daily. However, anakinra did not prevent the escalation of proteinuria following a URI. After the treatment was changed to adalimumab, a fully humanized monoclonal antibody to TNF-α, the patient continued to improve and reach full remission despite experiencing a cold and the flu in the following months.
Literature Review
There is a paucity of literature on applications of biological response modifiers for idiopathic NS and FSGS.23,24 Angeletti and colleagues reported that 3 patients with severe long-standing FSGS benefited from anakinra 4 mg/kg daily to reduce proteinuria and improve kidney function. All the patients had positive C3 staining in renal biopsy and treatment response, which supported the role of C3a in inducing podocyte injury through upregulated expression of IL-1 and IL-1R.23 Trachtman and colleagues reported on the phase II FONT trial that included 14 of 21 patients aged < 18 years with advanced FSGS who were treated with adalimumab 24 mg/m2, or ≤ 40 mg every other week.24 Although, during a 6-month period, none of the 7 patients met the endpoint of reduced proteinuria by ≥ 50%, and the authors suggested that careful patient selection may improve the treatment response in future trials.24
A recent study involving transcriptomics on renal tissue samples combined with available pathology (fibrosis), urinary markers, and clinical characteristics on 285 patients with MCD or FSGS from 3 different continents identified 3 distinct clusters. Patients with evidence of activated kidney TNF pathway (n = 72, aged > 18 years) were found to have poor clinical outcomes.25 The study identified 2 urine markers associated with the TNF pathway (ie, tissue inhibitor of metalloproteinases-1 and monocyte chemoattractant protein-1), which aligns with the preclinical findings previously mentioned.25
Conclusions
The patient’s condition in this case illustrates the complex nature of biologically predetermined cascading events in the emergence of glomerular disease upon environmental triggers under the influence of genetic factors.
Chronic kidney disease affects 7.7% of veterans annually, illustrating the need for new therapeutics.26 Based on our experience and literature review, upregulation of TNF-α is a root cause of glomerulopathy; further studies are warranted to evaluate the efficacy of anti-TNF biologic response modifiers for the treatment of these patients. Long-term postmarketing safety profile and steroid-sparing properties of adalimumab should allow inclusion of pediatric cases in future trials. Results may also contribute to identifying new predictive biomarkers related to the basement membrane when combined with precision nephrology to further advance patient selection and targeted treatment.25,27
Acknowledgments
The authors thank the patient’s mother for providing consent to allow publication of this case report.
1. Arif E, Nihalani D. Glomerular filtration barrier assembly: an insight. Postdoc J. 2013;1(4):33-45.
2. Garg PA. Review of podocyte biology. Am J Nephrol. 2018;47(suppl 1):3-13. doi:10.1159/000481633SUPPL
3. Warady BA, Agarwal R, Bangalore S, et al. Alport syndrome classification and management. Kidney Med. 2020;2(5):639-649. doi:10.1016/j.xkme.2020.05.014
4. Angioi A, Pani A. FSGS: from pathogenesis to the histological lesion. J Nephrol. 2016;29(4):517-523. doi:10.1007/s40620-016-0333-2
5. Roca N, Martinez C, Jatem E, Madrid A, Lopez M, Segarra A. Activation of the acute inflammatory phase response in idiopathic nephrotic syndrome: association with clinicopathological phenotypes and with response to corticosteroids. Clin Kidney J. 2021;14(4):1207-1215. doi:10.1093/ckj/sfaa247
6. Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal change disease. Clin J Am Soc Nephrol. 2017;12(2):332-345.
7. Medjeral-Thomas NR, Lawrence C, Condon M, et al. Randomized, controlled trial of tacrolimus and prednisolone monotherapy for adults with De Novo minimal change disease: a multicenter, randomized, controlled trial. Clin J Am Soc Nephrol. 2020;15(2):209-218. doi:10.2215/CJN.06290420
8. Ye Q, Lan B, Liu H, Persson PB, Lai EY, Mao J. A critical role of the podocyte cytoskeleton in the pathogenesis of glomerular proteinuria and autoimmune podocytopathies. Acta Physiol (Oxf). 2022;235(4):e13850. doi:10.1111/apha.13850
9. Trautmann A, Schnaidt S, Lipska-Ziμtkiewicz BS, et al. Long-term outcome of steroid-resistant nephrotic syndrome in children. J Am Soc Nephrol. 2017;28:3055-3065. doi:10.1681/ASN.2016101121
10. Kashtan CE, Gross O. Clinical practice recommendations for the diagnosis and management of Alport syndrome in children, adolescents, and young adults-an update for 2020. Pediatr Nephrol. 2021;36(3):711-719. doi:10.1007/s00467-020-04819-6
11. Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY. Thin basement membrane nephropathy. Kidney Int. 2003;64(4):1169-78. doi:10.1046/j.1523-1755.2003.00234.x
12. Rosenberg AZ, Kopp JB. Focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2017; 12(3):502-517. doi:10.2215/CJN.05960616
13. Savige J. Should we diagnose autosomal dominant Alport syndrome when there is a pathogenic heterozygous COL4A3 or COL4A4 variant? Kidney Int Rep. 2018;3(6):1239-1241. doi:10.1016/j.ekir.2018.08.002
14. Gigante M, Caridi G, Montemurno E, et al. TRPC6 mutations in children with steroid-resistant nephrotic syndrome and atypical phenotype. Clin J Am Soc Nephrol. 2011;6(7):1626-1634. doi:10.2215/CJN.07830910
15. Saurus P, Kuusela S, Lehtonen E, et al. Podocyte apoptosis is prevented by blocking the toll-like receptor pathway. Cell Death Dis. 2015;6(5):e1752. doi:10.1038/cddis.2015.125
16. Baud L, Oudinet JP, Bens M, et al. Production of tumor necrosis factor by rat mesangial cells in response to bacterial lipopolysaccharide. Kidney Int. 1989;35(5):1111-1118. doi:10.1038/ki.1989.98
17. White S, Lin L, Hu K. NF-κB and tPA signaling in kidney and other diseases. Cells. 2020;9(6):1348. doi:10.3390/cells9061348
18. Tesch GH, Lan HY, Atkins RC, Nikolic-Paterson DJ. Role of interleukin-1 in mesangial cell proliferation and matrix deposition in experimental mesangioproliferative nephritis. Am J Pathol. 1997;151(1):141-150.
19. Lai KN, Leung JCK, Chan LYY, et al. Podocyte injury induced by mesangial-derived cytokines in IgA Nephropathy. Nephrol Dial Transplant. 2009;24(1):62-72. doi:10.1093/ndt/gfn441
20. Saleem MA, Kobayashi Y. Cell biology and genetics of minimal change disease. F1000 Res. 2016;5: F1000 Faculty Rev-412. doi:10.12688/f1000research.7300.1
21. Kim KP, Williams CE, Lemmon CA. Cell-matrix interactions in renal fibrosis. Kidney Dial. 2022;2(4):607-624. doi:10.3390/kidneydial2040055
22. Zvaifler NJ. Relevance of the stroma and epithelial-mesenchymal transition (EMT) for the rheumatic diseases. Arthritis Res Ther. 2006;8(3):210. doi:10.1186/ar1963
23. Angeletti A, Magnasco A, Trivelli A, et al. Refractory minimal change disease and focal segmental glomerular sclerosis treated with Anakinra. Kidney Int Rep. 2021;7(1):121-124. doi:10.1016/j.ekir.2021.10.018
24. Trachtman H, Vento S, Herreshoff E, et al. Efficacy of galactose and adalimumab in patients with resistant focal segmental glomerulosclerosis: report of the font clinical trial group. BMC Nephrol. 2015;16:111. doi:10.1186/s12882-015-0094-5
25. Mariani LH, Eddy S, AlAkwaa FM, et al. Precision nephrology identified tumor necrosis factor activation variability in minimal change disease and focal segmental glomerulosclerosis. Kidney Int. 2023;103(3):565-579. doi:10.1016/j.kint.2022.10.023
26. Korshak L, Washington DL, Powell J, Nylen E, Kokkinos P. Kidney Disease in Veterans. US Dept of Veterans Affairs, Office of Health Equity. Updated May 13, 2020. Accessed June 28, 2024. https://www.va.gov/HEALTHEQUITY/Kidney_Disease_In_Veterans.asp
27. Malone AF, Phelan PJ, Hall G, et al. Rare hereditary COL4A3/COL4A4 variants may be mistaken for familial focal segmental glomerulosclerosis. Kidney Int. 2014;86(6):1253-1259. doi:10.1038/ki.2014.305
1. Arif E, Nihalani D. Glomerular filtration barrier assembly: an insight. Postdoc J. 2013;1(4):33-45.
2. Garg PA. Review of podocyte biology. Am J Nephrol. 2018;47(suppl 1):3-13. doi:10.1159/000481633SUPPL
3. Warady BA, Agarwal R, Bangalore S, et al. Alport syndrome classification and management. Kidney Med. 2020;2(5):639-649. doi:10.1016/j.xkme.2020.05.014
4. Angioi A, Pani A. FSGS: from pathogenesis to the histological lesion. J Nephrol. 2016;29(4):517-523. doi:10.1007/s40620-016-0333-2
5. Roca N, Martinez C, Jatem E, Madrid A, Lopez M, Segarra A. Activation of the acute inflammatory phase response in idiopathic nephrotic syndrome: association with clinicopathological phenotypes and with response to corticosteroids. Clin Kidney J. 2021;14(4):1207-1215. doi:10.1093/ckj/sfaa247
6. Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal change disease. Clin J Am Soc Nephrol. 2017;12(2):332-345.
7. Medjeral-Thomas NR, Lawrence C, Condon M, et al. Randomized, controlled trial of tacrolimus and prednisolone monotherapy for adults with De Novo minimal change disease: a multicenter, randomized, controlled trial. Clin J Am Soc Nephrol. 2020;15(2):209-218. doi:10.2215/CJN.06290420
8. Ye Q, Lan B, Liu H, Persson PB, Lai EY, Mao J. A critical role of the podocyte cytoskeleton in the pathogenesis of glomerular proteinuria and autoimmune podocytopathies. Acta Physiol (Oxf). 2022;235(4):e13850. doi:10.1111/apha.13850
9. Trautmann A, Schnaidt S, Lipska-Ziμtkiewicz BS, et al. Long-term outcome of steroid-resistant nephrotic syndrome in children. J Am Soc Nephrol. 2017;28:3055-3065. doi:10.1681/ASN.2016101121
10. Kashtan CE, Gross O. Clinical practice recommendations for the diagnosis and management of Alport syndrome in children, adolescents, and young adults-an update for 2020. Pediatr Nephrol. 2021;36(3):711-719. doi:10.1007/s00467-020-04819-6
11. Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY. Thin basement membrane nephropathy. Kidney Int. 2003;64(4):1169-78. doi:10.1046/j.1523-1755.2003.00234.x
12. Rosenberg AZ, Kopp JB. Focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2017; 12(3):502-517. doi:10.2215/CJN.05960616
13. Savige J. Should we diagnose autosomal dominant Alport syndrome when there is a pathogenic heterozygous COL4A3 or COL4A4 variant? Kidney Int Rep. 2018;3(6):1239-1241. doi:10.1016/j.ekir.2018.08.002
14. Gigante M, Caridi G, Montemurno E, et al. TRPC6 mutations in children with steroid-resistant nephrotic syndrome and atypical phenotype. Clin J Am Soc Nephrol. 2011;6(7):1626-1634. doi:10.2215/CJN.07830910
15. Saurus P, Kuusela S, Lehtonen E, et al. Podocyte apoptosis is prevented by blocking the toll-like receptor pathway. Cell Death Dis. 2015;6(5):e1752. doi:10.1038/cddis.2015.125
16. Baud L, Oudinet JP, Bens M, et al. Production of tumor necrosis factor by rat mesangial cells in response to bacterial lipopolysaccharide. Kidney Int. 1989;35(5):1111-1118. doi:10.1038/ki.1989.98
17. White S, Lin L, Hu K. NF-κB and tPA signaling in kidney and other diseases. Cells. 2020;9(6):1348. doi:10.3390/cells9061348
18. Tesch GH, Lan HY, Atkins RC, Nikolic-Paterson DJ. Role of interleukin-1 in mesangial cell proliferation and matrix deposition in experimental mesangioproliferative nephritis. Am J Pathol. 1997;151(1):141-150.
19. Lai KN, Leung JCK, Chan LYY, et al. Podocyte injury induced by mesangial-derived cytokines in IgA Nephropathy. Nephrol Dial Transplant. 2009;24(1):62-72. doi:10.1093/ndt/gfn441
20. Saleem MA, Kobayashi Y. Cell biology and genetics of minimal change disease. F1000 Res. 2016;5: F1000 Faculty Rev-412. doi:10.12688/f1000research.7300.1
21. Kim KP, Williams CE, Lemmon CA. Cell-matrix interactions in renal fibrosis. Kidney Dial. 2022;2(4):607-624. doi:10.3390/kidneydial2040055
22. Zvaifler NJ. Relevance of the stroma and epithelial-mesenchymal transition (EMT) for the rheumatic diseases. Arthritis Res Ther. 2006;8(3):210. doi:10.1186/ar1963
23. Angeletti A, Magnasco A, Trivelli A, et al. Refractory minimal change disease and focal segmental glomerular sclerosis treated with Anakinra. Kidney Int Rep. 2021;7(1):121-124. doi:10.1016/j.ekir.2021.10.018
24. Trachtman H, Vento S, Herreshoff E, et al. Efficacy of galactose and adalimumab in patients with resistant focal segmental glomerulosclerosis: report of the font clinical trial group. BMC Nephrol. 2015;16:111. doi:10.1186/s12882-015-0094-5
25. Mariani LH, Eddy S, AlAkwaa FM, et al. Precision nephrology identified tumor necrosis factor activation variability in minimal change disease and focal segmental glomerulosclerosis. Kidney Int. 2023;103(3):565-579. doi:10.1016/j.kint.2022.10.023
26. Korshak L, Washington DL, Powell J, Nylen E, Kokkinos P. Kidney Disease in Veterans. US Dept of Veterans Affairs, Office of Health Equity. Updated May 13, 2020. Accessed June 28, 2024. https://www.va.gov/HEALTHEQUITY/Kidney_Disease_In_Veterans.asp
27. Malone AF, Phelan PJ, Hall G, et al. Rare hereditary COL4A3/COL4A4 variants may be mistaken for familial focal segmental glomerulosclerosis. Kidney Int. 2014;86(6):1253-1259. doi:10.1038/ki.2014.305
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
Elusive Edema: A Case of Nephrotic Syndrome Mimicking Decompensated Cirrhosis
Elusive Edema: A Case of Nephrotic Syndrome Mimicking Decompensated Cirrhosis
Histology is the gold standard for cirrhosis diagnosis. However, a combination of clinical history, physical examination findings, and supportive laboratory and radiographic features is generally sufficient to make the diagnosis. Routine ultrasound and computed tomography (CT) imaging often identifies a nodular liver contour with sequelae of portal hypertension, including splenomegaly, varices, and ascites, which can suggest cirrhosis when supported by laboratory parameters and clinical features. As a result, the diagnosis is typically made clinically.1 Many patients with compensated cirrhosis go undetected. The presence of a decompensation event (ascites, spontaneous bacterial peritonitis, variceal hemorrhage, or hepatic encephalopathy) often leads to index diagnosis when patients were previously compensated. When a patient presents with suspected decompensated cirrhosis, it is important to consider other diagnoses with similar presentations and ensure that multiple disease processes are not contributing to the symptoms.
CASE PRESENTATION
A 64-year-old male with a history of intravenous (IV) methamphetamine use and prior incarceration presented with a 3-week history of progressively worsening generalized swelling. Prior to the onset of his symptoms, the patient injured his right lower extremity (RLE) in a bicycle accident, resulting in edema that progressed to bilateral lower extremity (BLE) edema and worsening fatigue, despite resolution of the initial injury. The patient gained weight though he could not quantify the amount. He experienced progressive hunger, thirst, and fatigue as well as increased sleep. Additionally, the patient experienced worsening dyspnea on exertion and orthopnea. He started using 2 pillows instead of 1 pillow at night.
The patient reported no fevers, chills, sputum production, chest pain, or paroxysmal nocturnal dyspnea. He had no known history of sexually transmitted infections, no significant history of alcohol use, and occasional tobacco and marijuana use. He had been incarcerated > 10 years before and last used IV methamphetamine 3 years before. He did not regularly take any medications.
The patient’s vital signs included a temperature of 98.2 °F; 78/min heart rate; 15/min respiratory rate; 159/109 mm Hg blood pressure; and 98% oxygen saturation on room air. He had gained 20 lbs in the past 4 months. He had pitting edema in both legs and arms, as well as periorbital swelling, but no jugular venous distention, abnormal heart sounds, or murmurs. Breath sounds were distant but clear to auscultation. His abdomen was distended with normal bowel sounds and no fluid wave; mild epigastric tenderness was present, but no intra-abdominal masses were palpated. He had spider angiomata on the upper chest but no other stigmata of cirrhosis, such as caput medusae or jaundice. Tattoos were noted.
Laboratory test results showed a platelet count of 178 x 103/μL (reference range, 140- 440 ~ 103μL).Creatinine was 0.80 mg/dL (reference range, < 1.28 mg/dL), with an estimated glomerular filtration rate (eGFR) of 99 mL/min/1.73 m2 using the Chronic Kidney Disease-Epidemiology equation (reference range, > 60 mL/min/1.73 m2), (reference range, > 60 mL/min/1.73 m2), and Cystatin C was 1.14 mg/L (reference range, < 1.15 mg/L). His electrolytes and complete blood count were within normal limits, including sodium, 134 mmol/L; potassium, 4.4 mmol/L; chloride, 108 mmol/L; and carbon dioxide, 22.5 mmol/L.
Additional test results included alkaline phosphatase, 126 U/L (reference range, < 94 U/L); alanine transaminase, 41 U/L (reference range, < 45 U/L); aspartate aminotransferase, 70 U/L (reference range, < 35 U/L); total bilirubin, 0.6 mg/dL (reference range, < 1 mg/dL); albumin, 1.8 g/dL (reference range, 3.2-4.8 g/dL); and total protein, 6.3 g/dL (reference range, 5.9-8.3 g/dL). The patient’s international normalized ratio was 0.96 (reference range, 0.8-1.1), and brain natriuretic peptide was normal at 56 pg/mL. No prior laboratory results were available for comparison.
Urine toxicology was positive for amphetamines. Urinalysis demonstrated large occult blood, with a red blood cell count of 26/ HPF (reference range, 0/HPF) and proteinuria (100 mg/dL; reference range, negative), without bacteria, nitrites, or leukocyte esterase. Urine white blood cell count was 10/ HPF (reference range, 0/HPF), and fine granular casts and hyaline casts were present.
A noncontrast CT of the abdomen and pelvis in the emergency department showed an irregular liver contour with diffuse nodularity, multiple portosystemic collaterals, moderate abdominal and pelvic ascites, small bilateral pleural effusions with associated atelectasis, and anasarca consistent with cirrhosis (Figure 1). The patient was admitted to the internal medicine service for workup and management of newly diagnosed cirrhosis.
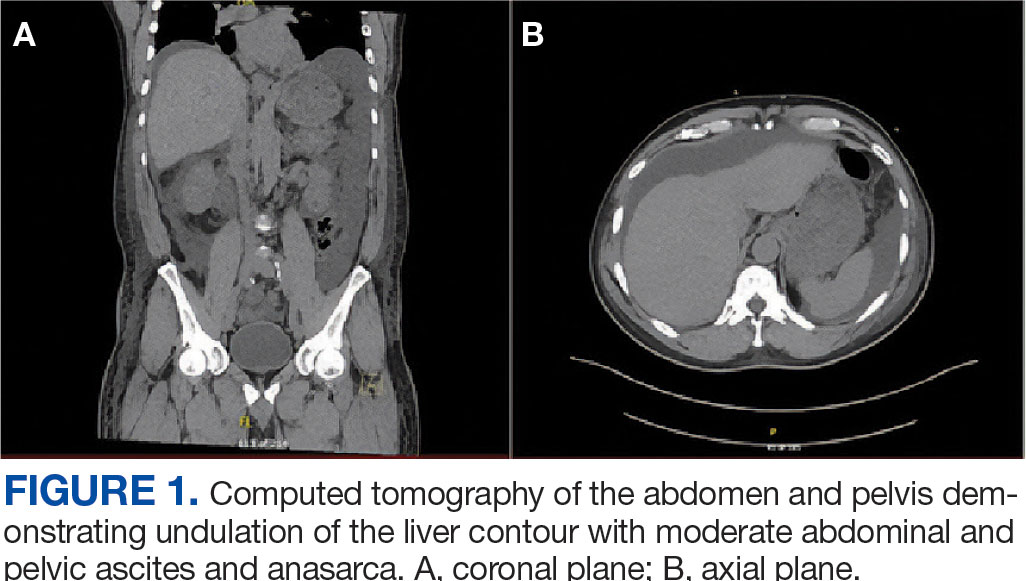
Paracentesis revealed straw-colored fluid with an ascitic fluid neutrophil count of 17/μL, a protein level of < 3 g/dL and albumin level of < 1.5 g/dL. Gram stain of the ascitic fluid showed a moderate white blood cell count with no organisms. Fluid culture showed no microbial growth.
Initial workup for cirrhosis demonstrated a positive total hepatitis A antibody. The patient had a nonreactive hepatitis B surface antigen and surface antibody, but a reactive hepatitis B core antibody; a hepatitis B DNA level was not ordered. He had a reactive hepatitis C antibody with a viral load of 4,490,000 II/mL (genotype 1a). The patient’s iron level was 120 μg/dL, with a calculated total iron-binding capacity (TIBC) of 126.2 μg/dL. His transferrin saturation (TSAT) (serum iron divided by TIBC) was 95%. The patient had nonreactive antinuclear antibody and antimitochondrial antibody tests and a positive antismooth muscle antibody test with a titer of 1:40. His α-fetoprotein (AFP) level was 505 ng/mL (reference range, < 8 ng/mL).
Follow-up MRI of the abdomen and pelvis showed cirrhotic morphology with large volume ascites and portosystemic collaterals, consistent with portal hypertension. Additionally, it showed multiple scattered peripheral sub centimeter hyperenhancing foci, most likely representing benign lesions.
The patient's spot urine protein-creatinine ratio was 3.76. To better quantify proteinuria, a 24-hour urine collection was performed and revealed 12.8 g/d of urine protein (reference range, 0-0.17 g/d). His serum triglyceride level was 175 mg/dL (reference range, 40-60 mg/dL); total cholesterol was 177 mg/ dL (reference range, ≤ 200 mg/dL); low density lipoprotein cholesterol was 98 mg/ dL (reference range, ≤ 130 mg/dL); and highdensity lipoprotein cholesterol was 43.8 mg/ dL (reference range, ≥ 40 mg/dL); C3 complement level was 71 mg/dL (reference range, 82-185 mg/dL); and C4 complement level was 22 mg/dL (reference range, 15-53 mg/ dL). His rheumatoid factor was < 14 IU/mL. Tests for rapid plasma reagin and HIV antigen- antibody were nonreactive, and the phospholipase A2 receptor antibody test was negative. The patient tested positive for QuantiFERON-TB Gold and qualitative cryoglobulin, which indicated a cryocrit of 1%.
A renal biopsy was performed, revealing diffuse podocyte foot process effacement and glomerulonephritis with low-grade C3 and immunoglobulin (Ig) G deposits, consistent with early membranoproliferative glomerulonephritis (MPGN) (Figures 2 and 3).
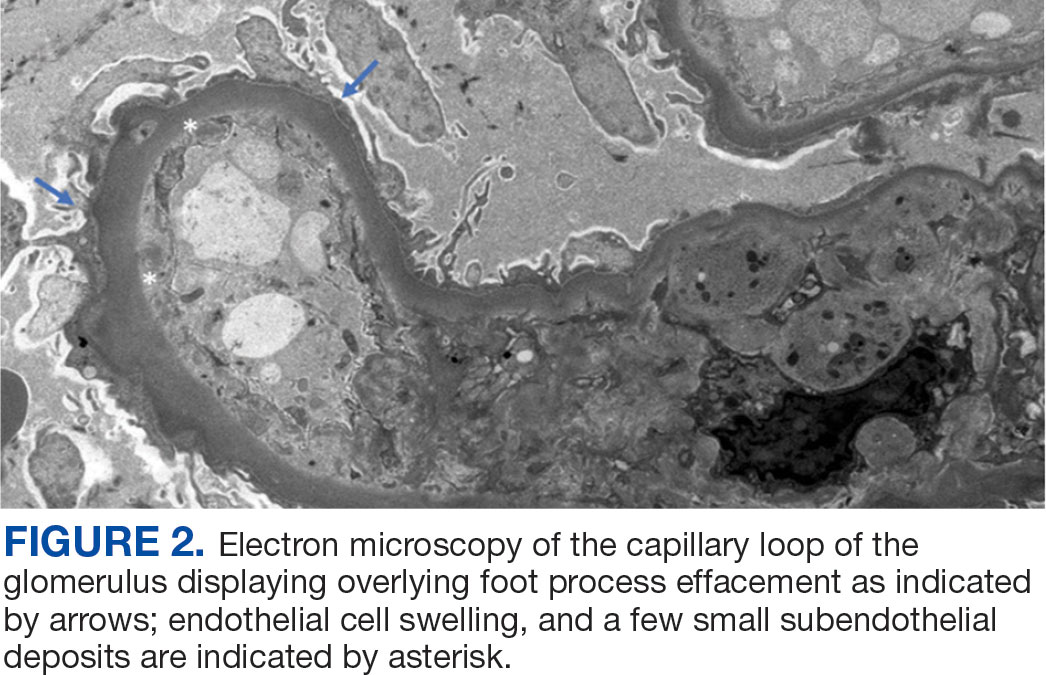
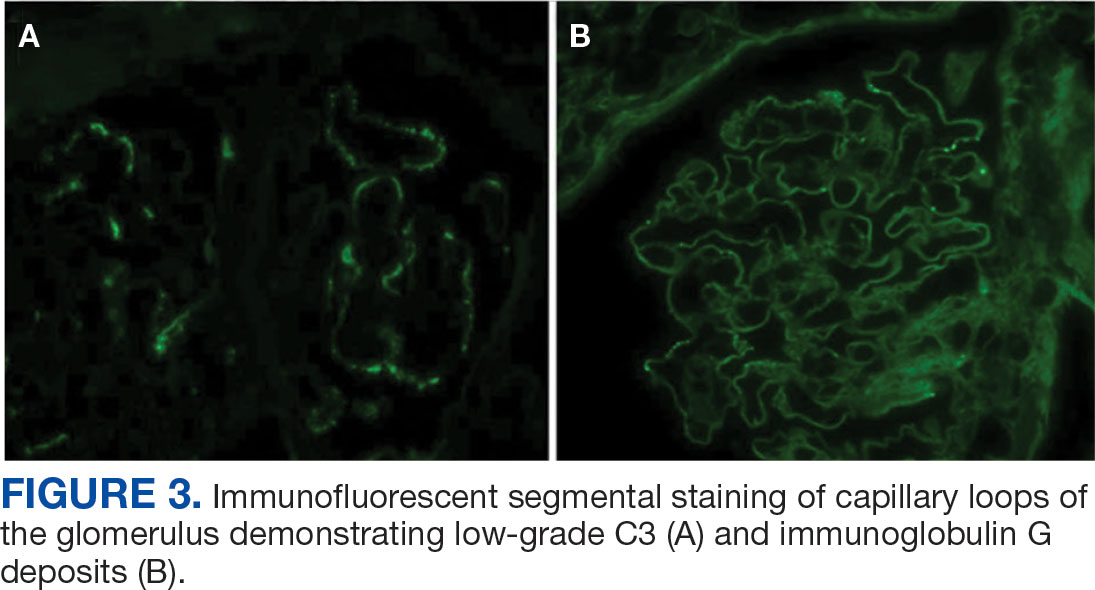
The patient was initially diuresed with IV furosemide without significant urine output. He was then diuresed with IV 25% albumin (total, 25 g), followed by IV furosemide 40 mg twice daily, which led to significant urine output and resolution of his anasarca. Given the patient’s hypoalbuminemic state, IV albumin was necessary to deliver furosemide to the proximal tubule. He was started on lisinopril for renal protection and discharged with spironolactone and furosemide for fluid management in the context of cirrhosis.
The patient was evaluated by the Liver Nodule Clinic, which includes specialists from hepatology, medical oncology, radiation oncology, interventional radiology, and diagnostic radiology. The team considered the patient’s medical history and characteristics of the nodules on imaging. Notable aspects of the patient’s history included hepatitis C virus (HCV) infection and an elevated AFP level, although imaging showed no lesion concerning for malignancy. Given these findings, the patient was scheduled for a liver biopsy to establish a tissue diagnosis of cirrhosis. Hepatology, nephrology, and infectious disease specialists coordinated to plan the management and treatment of latent tuberculosis (TB), chronic HCV, MPGN, compensated cirrhosis, and suspicious liver lesions.
The patient chose to handle management and treatment as an outpatient. He was discharged with furosemide and spironolactone for anasarca management, and amlodipine and lisinopril for his hypertension and MPGN. Follow-up appointments were scheduled with infectious disease for management of latent TB and HCV, nephrology for MPGN, gastroenterology for cirrhosis, and interventional radiology for liver biopsy. Unfortunately, the patient was unhoused with limited access to transportation, which prevented timely follow-up. Given these social factors, immunosuppression was not started. Additionally, he did not start on HCV therapy because the viral load was still pending at time of discharge.
DISCUSSION
The diagnosis of decompensated cirrhosis was prematurely established, resulting in a diagnostic delay, a form of diagnostic error. However, on hospital day 2, the initial hypothesis of decompensated cirrhosis as the sole driver of the patient’s presentation was reconsidered due to the disconnect between the severity of hypoalbuminemia and diffuse edema (anasarca), and the absence of laboratory evidence of hepatic decompensation (normal international normalized ratio, bilirubin, and low but normal platelet count). Although image findings supported cirrhosis, laboratory markers did not indicate hepatic decompensation. The severity of hypoalbuminemia and anasarca, along with an indeterminate Serum-Ascites Albumin Gradient, prompted the patient’s care team to consider other causes, specifically, nephrotic syndrome.
The patien’s spot protein-to-creatinine ratio was 3.76 (reference range < 0.2 mg/mg creatinine), but a 24-hour urine protein collection was 12.8 g/day (reference range < 150 mg/day). While most spot urine protein- to-creatinine ratios (UPCR) correlate with a 24-hour urine collection, discrepancies can occur, as in this case. It is important to recognize that the spot UPCR assumes that patients are excreting 1000 mg of creatinine daily in their urine, which is not always the case. In addition, changes in urine osmolality can lead to different values. The gold standard for proteinuria is a 24-hour urine collection for protein and creatinine.
The patient’s nephrotic-range proteinuria and severe hypoalbuminemia are not solely explained by cirrhosis. In addition, the patient’s lower extremity edema pointed to nephrotic syndrome. The differential diagnosis for nephrotic syndrome includes both primary and secondary forms of membranous nephropathy, minimal change disease, focal segmental glomerulosclerosis, and MPGN, a histopathological diagnosis that requires distinguishing between immune complex-mediated and complement-mediated forms. Other causes of nephrotic syndrome that do not fit in any of these buckets include amyloidosis, IgA nephropathy, and diabetes mellitus (DM). Despite DM being a common cause of nephrotic range proteinuria, it rarely leads to full nephrotic syndrome.
When considering the diagnosis, we reframed the patient’s clinical syndrome as compensated cirrhosis plus nephrotic syndrome. This approach prioritized identifying a cause that could explain both cirrhosis (from any cause) leading to IgA nephropathy or injection drug use serving as a risk factor for cirrhosis and nephrotic syndrome through HCV or AA amyloidosis, respectively. This problem representation guided us to the correct diagnosis. There are multiple renal diseases associated with HCV infection, including MPGN, membranous nephropathy, focal segmental glomerulosclerosis, and IgA nephropathy.2 MPGN and mixed cryoglobulinemia are the most common. In the past, MPGN was classified as type I, II, and III.
The patient’s urine toxicology revealed recent amphetamine use, which can also lead to acute kidney injury through rhabdomyolysis or acute interstitial nephritis (AIN).3 In the cases of rhabdomyolysis, urinalysis would show positive heme without any red blood cell on microscopic analysis, which was not present in this case. AIN commonly manifests as acute kidney injury, pyuria, and proteinuria but without a decrease in complement levels.4 While the patient’s urine sediment included white blood cell (10/high-power field), the presence of microscopic hematuria, decreased complement levels, and proteinuria in the context of HCV positivity makes MPGN more likely than AIN.
Recently, there has been greater emphasis on using immunofluorescence for kidney biopsies. MPGN is now classified into 2 main categories: MPGN with mesangial immunoglobulins and C3 deposits in the capillary walls, and MPGN with C3 deposits but without Ig.5 MPGN with Ig-complement deposits is seen in autoimmune diseases and infections and is associated with dysproteinemias.
The renal biopsy in this patient was consistent with MPGN with immunofluorescence, a common finding in patients with infection. By synthesizing these data, we concluded that the patient represented a case of chronic HCV infection that led to MPGN with cryoglobulinemia. The normal C4 and negative RF do not suggest cryoglobulinemic crisis. Compensated cirrhosis was seen on imaging, pending liver biopsy.
Treatment
The management of MPGN secondary to HCV infection relies on the treatment of the underlying infection and clearance of viral load. Direct-acting antivirals have been used successfully in the treatment of HCV-associated MPGN. When cryoglobulinemia is present, immunosuppressive therapy is recommended. These regimens commonly include rituximab and steroids.5 Rituximab is also used for nephrotic syndrome associated with MPGN, as recommended in the 2018 Kidney Disease: Improving Global Outcomes guidelines.6
When initiating rituximab therapy in a patient who tests positive for hepatitis B (HBcAb positive or HBsAb positive), it is recommended to follow the established guidelines, which include treating them with entecavir for prophylaxis to prevent reactivation or a flare of hepatitis B.7 The patient in this case needed close follow-up in the nephrology and hepatology clinic. Immunosuppressive therapy was not pursued while the patient was admitted to the hospital due to instability with housing, transportation, and difficulty in ensuring close follow-up.
CONCLUSIONS
Clinicians should maintain a broad differential even in the face of confirmatory imaging and other objective findings. In the case of anasarca, nephrotic syndrome should be considered. Key causes of nephrotic syndromes include MPGN, membranous nephropathy, minimal change disease, and focal segmental glomerulosclerosis. MPGN is a histopathological diagnosis, and it is essential to identify if it is secondary to immune complexes or only complement mediated because Ig-complement deposits are seen in autoimmune disease and infection. The management of MPGN due to HCV infection relies on antiviral therapy. In the presence of cryoglobulinemia, immunosuppressive therapy is recommended.
- Tapper EB, Parikh ND. Diagnosis and management of cirrhosis and its complications: a review. JAMA. 2023;329(18):1589–1602. doi:10.1001/jama.2023.5997
- Ozkok A, Yildiz A. Hepatitis C virus associated glomerulopathies. World J Gastroenterol. 2014;20(24):7544-7554. doi:10.3748/wjg.v20.i24.7544
- Foley RJ, Kapatkin K, Vrani R, Weinman EJ. Amphetamineinduced acute renal failure. South Med J. 1984;77(2):258- 260. doi:10.1097/00007611-198402000-00035
- Rossert J. Drug - induced acute interstitial nephritis. Kidney Int. 2001;60(2):804-817. doi:10.1046/j.1523-1755.2001.060002804.x
- Sethi S, Fervenza FC. Membranoproliferative glomerulonephritis: pathogenetic heterogeneity and proposal for a new classification. Semin Nephrol. 2011;31(4):341-348. doi:10.1016/j.semnephrol.2011.06.005
- Jadoul M, Berenguer MC, Doss W, et al. Executive summary of the 2018 KDIGO hepatitis C in CKD guideline: welcoming advances in evaluation and management. Kidney Int. 2018;94(4):663-673. doi:10.1016/j.kint.2018.06.011
- Myint A, Tong MJ, Beaven SW. Reactivation of hepatitis b virus: a review of clinical guidelines. Clin Liver Dis (Hoboken). 2020;15(4):162-167. doi:10.1002/cld.883
Histology is the gold standard for cirrhosis diagnosis. However, a combination of clinical history, physical examination findings, and supportive laboratory and radiographic features is generally sufficient to make the diagnosis. Routine ultrasound and computed tomography (CT) imaging often identifies a nodular liver contour with sequelae of portal hypertension, including splenomegaly, varices, and ascites, which can suggest cirrhosis when supported by laboratory parameters and clinical features. As a result, the diagnosis is typically made clinically.1 Many patients with compensated cirrhosis go undetected. The presence of a decompensation event (ascites, spontaneous bacterial peritonitis, variceal hemorrhage, or hepatic encephalopathy) often leads to index diagnosis when patients were previously compensated. When a patient presents with suspected decompensated cirrhosis, it is important to consider other diagnoses with similar presentations and ensure that multiple disease processes are not contributing to the symptoms.
CASE PRESENTATION
A 64-year-old male with a history of intravenous (IV) methamphetamine use and prior incarceration presented with a 3-week history of progressively worsening generalized swelling. Prior to the onset of his symptoms, the patient injured his right lower extremity (RLE) in a bicycle accident, resulting in edema that progressed to bilateral lower extremity (BLE) edema and worsening fatigue, despite resolution of the initial injury. The patient gained weight though he could not quantify the amount. He experienced progressive hunger, thirst, and fatigue as well as increased sleep. Additionally, the patient experienced worsening dyspnea on exertion and orthopnea. He started using 2 pillows instead of 1 pillow at night.
The patient reported no fevers, chills, sputum production, chest pain, or paroxysmal nocturnal dyspnea. He had no known history of sexually transmitted infections, no significant history of alcohol use, and occasional tobacco and marijuana use. He had been incarcerated > 10 years before and last used IV methamphetamine 3 years before. He did not regularly take any medications.
The patient’s vital signs included a temperature of 98.2 °F; 78/min heart rate; 15/min respiratory rate; 159/109 mm Hg blood pressure; and 98% oxygen saturation on room air. He had gained 20 lbs in the past 4 months. He had pitting edema in both legs and arms, as well as periorbital swelling, but no jugular venous distention, abnormal heart sounds, or murmurs. Breath sounds were distant but clear to auscultation. His abdomen was distended with normal bowel sounds and no fluid wave; mild epigastric tenderness was present, but no intra-abdominal masses were palpated. He had spider angiomata on the upper chest but no other stigmata of cirrhosis, such as caput medusae or jaundice. Tattoos were noted.
Laboratory test results showed a platelet count of 178 x 103/μL (reference range, 140- 440 ~ 103μL).Creatinine was 0.80 mg/dL (reference range, < 1.28 mg/dL), with an estimated glomerular filtration rate (eGFR) of 99 mL/min/1.73 m2 using the Chronic Kidney Disease-Epidemiology equation (reference range, > 60 mL/min/1.73 m2), (reference range, > 60 mL/min/1.73 m2), and Cystatin C was 1.14 mg/L (reference range, < 1.15 mg/L). His electrolytes and complete blood count were within normal limits, including sodium, 134 mmol/L; potassium, 4.4 mmol/L; chloride, 108 mmol/L; and carbon dioxide, 22.5 mmol/L.
Additional test results included alkaline phosphatase, 126 U/L (reference range, < 94 U/L); alanine transaminase, 41 U/L (reference range, < 45 U/L); aspartate aminotransferase, 70 U/L (reference range, < 35 U/L); total bilirubin, 0.6 mg/dL (reference range, < 1 mg/dL); albumin, 1.8 g/dL (reference range, 3.2-4.8 g/dL); and total protein, 6.3 g/dL (reference range, 5.9-8.3 g/dL). The patient’s international normalized ratio was 0.96 (reference range, 0.8-1.1), and brain natriuretic peptide was normal at 56 pg/mL. No prior laboratory results were available for comparison.
Urine toxicology was positive for amphetamines. Urinalysis demonstrated large occult blood, with a red blood cell count of 26/ HPF (reference range, 0/HPF) and proteinuria (100 mg/dL; reference range, negative), without bacteria, nitrites, or leukocyte esterase. Urine white blood cell count was 10/ HPF (reference range, 0/HPF), and fine granular casts and hyaline casts were present.
A noncontrast CT of the abdomen and pelvis in the emergency department showed an irregular liver contour with diffuse nodularity, multiple portosystemic collaterals, moderate abdominal and pelvic ascites, small bilateral pleural effusions with associated atelectasis, and anasarca consistent with cirrhosis (Figure 1). The patient was admitted to the internal medicine service for workup and management of newly diagnosed cirrhosis.
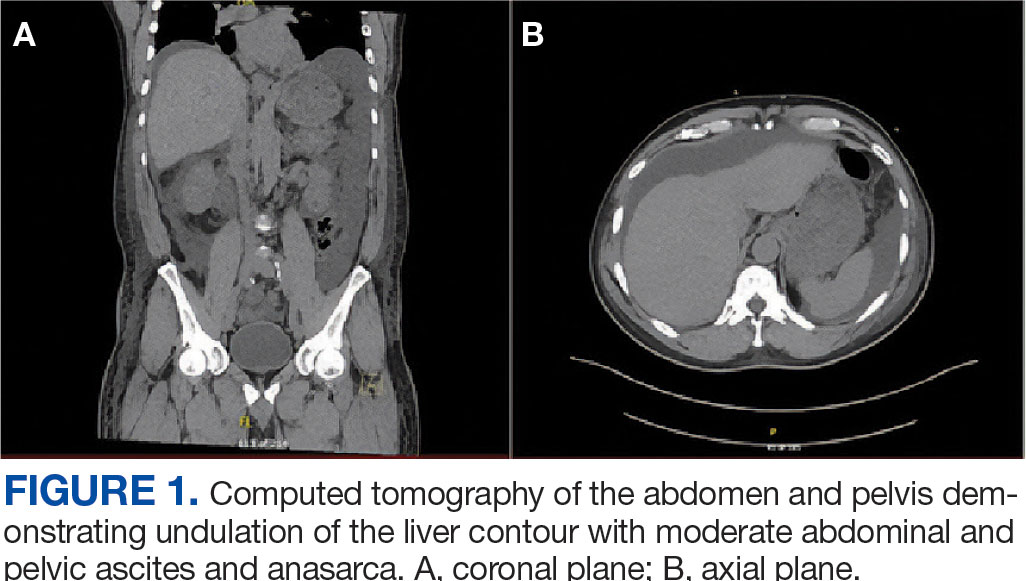
Paracentesis revealed straw-colored fluid with an ascitic fluid neutrophil count of 17/μL, a protein level of < 3 g/dL and albumin level of < 1.5 g/dL. Gram stain of the ascitic fluid showed a moderate white blood cell count with no organisms. Fluid culture showed no microbial growth.
Initial workup for cirrhosis demonstrated a positive total hepatitis A antibody. The patient had a nonreactive hepatitis B surface antigen and surface antibody, but a reactive hepatitis B core antibody; a hepatitis B DNA level was not ordered. He had a reactive hepatitis C antibody with a viral load of 4,490,000 II/mL (genotype 1a). The patient’s iron level was 120 μg/dL, with a calculated total iron-binding capacity (TIBC) of 126.2 μg/dL. His transferrin saturation (TSAT) (serum iron divided by TIBC) was 95%. The patient had nonreactive antinuclear antibody and antimitochondrial antibody tests and a positive antismooth muscle antibody test with a titer of 1:40. His α-fetoprotein (AFP) level was 505 ng/mL (reference range, < 8 ng/mL).
Follow-up MRI of the abdomen and pelvis showed cirrhotic morphology with large volume ascites and portosystemic collaterals, consistent with portal hypertension. Additionally, it showed multiple scattered peripheral sub centimeter hyperenhancing foci, most likely representing benign lesions.
The patient's spot urine protein-creatinine ratio was 3.76. To better quantify proteinuria, a 24-hour urine collection was performed and revealed 12.8 g/d of urine protein (reference range, 0-0.17 g/d). His serum triglyceride level was 175 mg/dL (reference range, 40-60 mg/dL); total cholesterol was 177 mg/ dL (reference range, ≤ 200 mg/dL); low density lipoprotein cholesterol was 98 mg/ dL (reference range, ≤ 130 mg/dL); and highdensity lipoprotein cholesterol was 43.8 mg/ dL (reference range, ≥ 40 mg/dL); C3 complement level was 71 mg/dL (reference range, 82-185 mg/dL); and C4 complement level was 22 mg/dL (reference range, 15-53 mg/ dL). His rheumatoid factor was < 14 IU/mL. Tests for rapid plasma reagin and HIV antigen- antibody were nonreactive, and the phospholipase A2 receptor antibody test was negative. The patient tested positive for QuantiFERON-TB Gold and qualitative cryoglobulin, which indicated a cryocrit of 1%.
A renal biopsy was performed, revealing diffuse podocyte foot process effacement and glomerulonephritis with low-grade C3 and immunoglobulin (Ig) G deposits, consistent with early membranoproliferative glomerulonephritis (MPGN) (Figures 2 and 3).
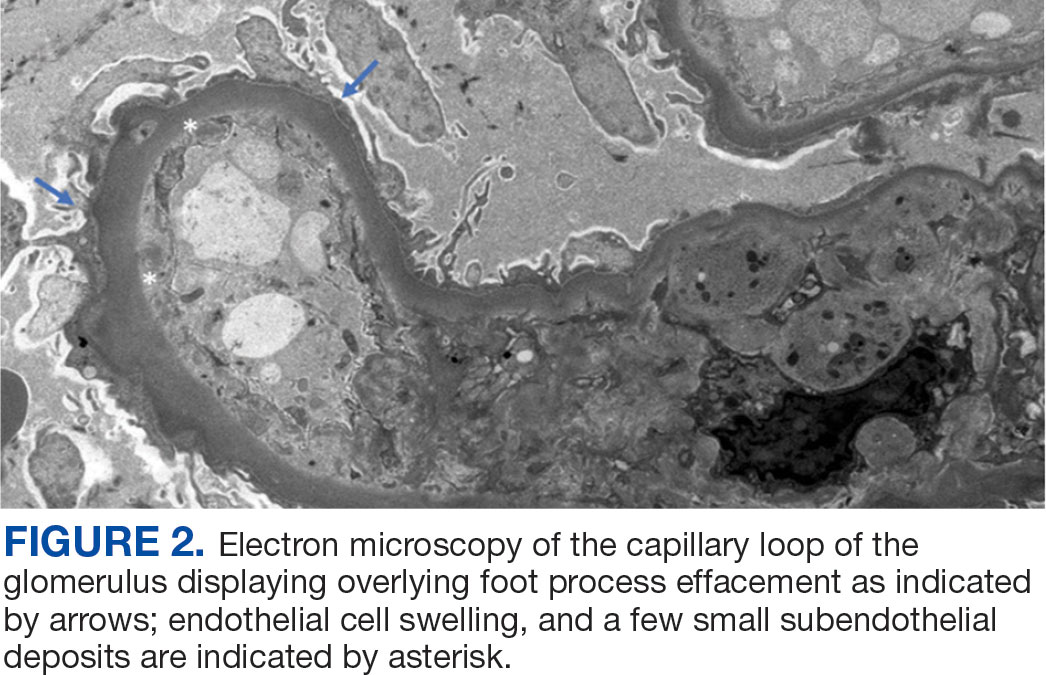
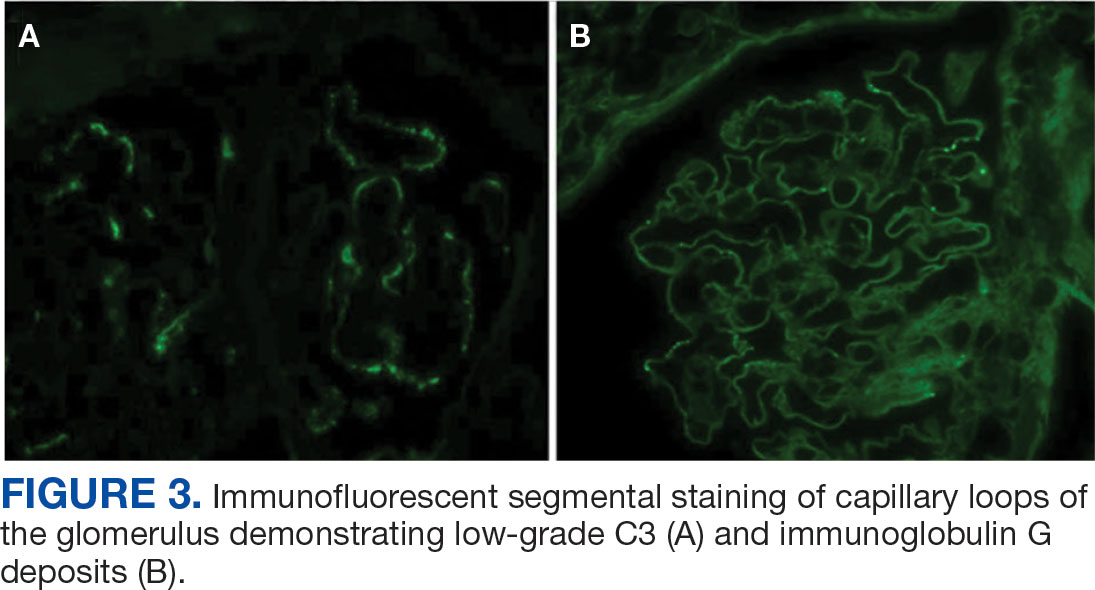
The patient was initially diuresed with IV furosemide without significant urine output. He was then diuresed with IV 25% albumin (total, 25 g), followed by IV furosemide 40 mg twice daily, which led to significant urine output and resolution of his anasarca. Given the patient’s hypoalbuminemic state, IV albumin was necessary to deliver furosemide to the proximal tubule. He was started on lisinopril for renal protection and discharged with spironolactone and furosemide for fluid management in the context of cirrhosis.
The patient was evaluated by the Liver Nodule Clinic, which includes specialists from hepatology, medical oncology, radiation oncology, interventional radiology, and diagnostic radiology. The team considered the patient’s medical history and characteristics of the nodules on imaging. Notable aspects of the patient’s history included hepatitis C virus (HCV) infection and an elevated AFP level, although imaging showed no lesion concerning for malignancy. Given these findings, the patient was scheduled for a liver biopsy to establish a tissue diagnosis of cirrhosis. Hepatology, nephrology, and infectious disease specialists coordinated to plan the management and treatment of latent tuberculosis (TB), chronic HCV, MPGN, compensated cirrhosis, and suspicious liver lesions.
The patient chose to handle management and treatment as an outpatient. He was discharged with furosemide and spironolactone for anasarca management, and amlodipine and lisinopril for his hypertension and MPGN. Follow-up appointments were scheduled with infectious disease for management of latent TB and HCV, nephrology for MPGN, gastroenterology for cirrhosis, and interventional radiology for liver biopsy. Unfortunately, the patient was unhoused with limited access to transportation, which prevented timely follow-up. Given these social factors, immunosuppression was not started. Additionally, he did not start on HCV therapy because the viral load was still pending at time of discharge.
DISCUSSION
The diagnosis of decompensated cirrhosis was prematurely established, resulting in a diagnostic delay, a form of diagnostic error. However, on hospital day 2, the initial hypothesis of decompensated cirrhosis as the sole driver of the patient’s presentation was reconsidered due to the disconnect between the severity of hypoalbuminemia and diffuse edema (anasarca), and the absence of laboratory evidence of hepatic decompensation (normal international normalized ratio, bilirubin, and low but normal platelet count). Although image findings supported cirrhosis, laboratory markers did not indicate hepatic decompensation. The severity of hypoalbuminemia and anasarca, along with an indeterminate Serum-Ascites Albumin Gradient, prompted the patient’s care team to consider other causes, specifically, nephrotic syndrome.
The patien’s spot protein-to-creatinine ratio was 3.76 (reference range < 0.2 mg/mg creatinine), but a 24-hour urine protein collection was 12.8 g/day (reference range < 150 mg/day). While most spot urine protein- to-creatinine ratios (UPCR) correlate with a 24-hour urine collection, discrepancies can occur, as in this case. It is important to recognize that the spot UPCR assumes that patients are excreting 1000 mg of creatinine daily in their urine, which is not always the case. In addition, changes in urine osmolality can lead to different values. The gold standard for proteinuria is a 24-hour urine collection for protein and creatinine.
The patient’s nephrotic-range proteinuria and severe hypoalbuminemia are not solely explained by cirrhosis. In addition, the patient’s lower extremity edema pointed to nephrotic syndrome. The differential diagnosis for nephrotic syndrome includes both primary and secondary forms of membranous nephropathy, minimal change disease, focal segmental glomerulosclerosis, and MPGN, a histopathological diagnosis that requires distinguishing between immune complex-mediated and complement-mediated forms. Other causes of nephrotic syndrome that do not fit in any of these buckets include amyloidosis, IgA nephropathy, and diabetes mellitus (DM). Despite DM being a common cause of nephrotic range proteinuria, it rarely leads to full nephrotic syndrome.
When considering the diagnosis, we reframed the patient’s clinical syndrome as compensated cirrhosis plus nephrotic syndrome. This approach prioritized identifying a cause that could explain both cirrhosis (from any cause) leading to IgA nephropathy or injection drug use serving as a risk factor for cirrhosis and nephrotic syndrome through HCV or AA amyloidosis, respectively. This problem representation guided us to the correct diagnosis. There are multiple renal diseases associated with HCV infection, including MPGN, membranous nephropathy, focal segmental glomerulosclerosis, and IgA nephropathy.2 MPGN and mixed cryoglobulinemia are the most common. In the past, MPGN was classified as type I, II, and III.
The patient’s urine toxicology revealed recent amphetamine use, which can also lead to acute kidney injury through rhabdomyolysis or acute interstitial nephritis (AIN).3 In the cases of rhabdomyolysis, urinalysis would show positive heme without any red blood cell on microscopic analysis, which was not present in this case. AIN commonly manifests as acute kidney injury, pyuria, and proteinuria but without a decrease in complement levels.4 While the patient’s urine sediment included white blood cell (10/high-power field), the presence of microscopic hematuria, decreased complement levels, and proteinuria in the context of HCV positivity makes MPGN more likely than AIN.
Recently, there has been greater emphasis on using immunofluorescence for kidney biopsies. MPGN is now classified into 2 main categories: MPGN with mesangial immunoglobulins and C3 deposits in the capillary walls, and MPGN with C3 deposits but without Ig.5 MPGN with Ig-complement deposits is seen in autoimmune diseases and infections and is associated with dysproteinemias.
The renal biopsy in this patient was consistent with MPGN with immunofluorescence, a common finding in patients with infection. By synthesizing these data, we concluded that the patient represented a case of chronic HCV infection that led to MPGN with cryoglobulinemia. The normal C4 and negative RF do not suggest cryoglobulinemic crisis. Compensated cirrhosis was seen on imaging, pending liver biopsy.
Treatment
The management of MPGN secondary to HCV infection relies on the treatment of the underlying infection and clearance of viral load. Direct-acting antivirals have been used successfully in the treatment of HCV-associated MPGN. When cryoglobulinemia is present, immunosuppressive therapy is recommended. These regimens commonly include rituximab and steroids.5 Rituximab is also used for nephrotic syndrome associated with MPGN, as recommended in the 2018 Kidney Disease: Improving Global Outcomes guidelines.6
When initiating rituximab therapy in a patient who tests positive for hepatitis B (HBcAb positive or HBsAb positive), it is recommended to follow the established guidelines, which include treating them with entecavir for prophylaxis to prevent reactivation or a flare of hepatitis B.7 The patient in this case needed close follow-up in the nephrology and hepatology clinic. Immunosuppressive therapy was not pursued while the patient was admitted to the hospital due to instability with housing, transportation, and difficulty in ensuring close follow-up.
CONCLUSIONS
Clinicians should maintain a broad differential even in the face of confirmatory imaging and other objective findings. In the case of anasarca, nephrotic syndrome should be considered. Key causes of nephrotic syndromes include MPGN, membranous nephropathy, minimal change disease, and focal segmental glomerulosclerosis. MPGN is a histopathological diagnosis, and it is essential to identify if it is secondary to immune complexes or only complement mediated because Ig-complement deposits are seen in autoimmune disease and infection. The management of MPGN due to HCV infection relies on antiviral therapy. In the presence of cryoglobulinemia, immunosuppressive therapy is recommended.
Histology is the gold standard for cirrhosis diagnosis. However, a combination of clinical history, physical examination findings, and supportive laboratory and radiographic features is generally sufficient to make the diagnosis. Routine ultrasound and computed tomography (CT) imaging often identifies a nodular liver contour with sequelae of portal hypertension, including splenomegaly, varices, and ascites, which can suggest cirrhosis when supported by laboratory parameters and clinical features. As a result, the diagnosis is typically made clinically.1 Many patients with compensated cirrhosis go undetected. The presence of a decompensation event (ascites, spontaneous bacterial peritonitis, variceal hemorrhage, or hepatic encephalopathy) often leads to index diagnosis when patients were previously compensated. When a patient presents with suspected decompensated cirrhosis, it is important to consider other diagnoses with similar presentations and ensure that multiple disease processes are not contributing to the symptoms.
CASE PRESENTATION
A 64-year-old male with a history of intravenous (IV) methamphetamine use and prior incarceration presented with a 3-week history of progressively worsening generalized swelling. Prior to the onset of his symptoms, the patient injured his right lower extremity (RLE) in a bicycle accident, resulting in edema that progressed to bilateral lower extremity (BLE) edema and worsening fatigue, despite resolution of the initial injury. The patient gained weight though he could not quantify the amount. He experienced progressive hunger, thirst, and fatigue as well as increased sleep. Additionally, the patient experienced worsening dyspnea on exertion and orthopnea. He started using 2 pillows instead of 1 pillow at night.
The patient reported no fevers, chills, sputum production, chest pain, or paroxysmal nocturnal dyspnea. He had no known history of sexually transmitted infections, no significant history of alcohol use, and occasional tobacco and marijuana use. He had been incarcerated > 10 years before and last used IV methamphetamine 3 years before. He did not regularly take any medications.
The patient’s vital signs included a temperature of 98.2 °F; 78/min heart rate; 15/min respiratory rate; 159/109 mm Hg blood pressure; and 98% oxygen saturation on room air. He had gained 20 lbs in the past 4 months. He had pitting edema in both legs and arms, as well as periorbital swelling, but no jugular venous distention, abnormal heart sounds, or murmurs. Breath sounds were distant but clear to auscultation. His abdomen was distended with normal bowel sounds and no fluid wave; mild epigastric tenderness was present, but no intra-abdominal masses were palpated. He had spider angiomata on the upper chest but no other stigmata of cirrhosis, such as caput medusae or jaundice. Tattoos were noted.
Laboratory test results showed a platelet count of 178 x 103/μL (reference range, 140- 440 ~ 103μL).Creatinine was 0.80 mg/dL (reference range, < 1.28 mg/dL), with an estimated glomerular filtration rate (eGFR) of 99 mL/min/1.73 m2 using the Chronic Kidney Disease-Epidemiology equation (reference range, > 60 mL/min/1.73 m2), (reference range, > 60 mL/min/1.73 m2), and Cystatin C was 1.14 mg/L (reference range, < 1.15 mg/L). His electrolytes and complete blood count were within normal limits, including sodium, 134 mmol/L; potassium, 4.4 mmol/L; chloride, 108 mmol/L; and carbon dioxide, 22.5 mmol/L.
Additional test results included alkaline phosphatase, 126 U/L (reference range, < 94 U/L); alanine transaminase, 41 U/L (reference range, < 45 U/L); aspartate aminotransferase, 70 U/L (reference range, < 35 U/L); total bilirubin, 0.6 mg/dL (reference range, < 1 mg/dL); albumin, 1.8 g/dL (reference range, 3.2-4.8 g/dL); and total protein, 6.3 g/dL (reference range, 5.9-8.3 g/dL). The patient’s international normalized ratio was 0.96 (reference range, 0.8-1.1), and brain natriuretic peptide was normal at 56 pg/mL. No prior laboratory results were available for comparison.
Urine toxicology was positive for amphetamines. Urinalysis demonstrated large occult blood, with a red blood cell count of 26/ HPF (reference range, 0/HPF) and proteinuria (100 mg/dL; reference range, negative), without bacteria, nitrites, or leukocyte esterase. Urine white blood cell count was 10/ HPF (reference range, 0/HPF), and fine granular casts and hyaline casts were present.
A noncontrast CT of the abdomen and pelvis in the emergency department showed an irregular liver contour with diffuse nodularity, multiple portosystemic collaterals, moderate abdominal and pelvic ascites, small bilateral pleural effusions with associated atelectasis, and anasarca consistent with cirrhosis (Figure 1). The patient was admitted to the internal medicine service for workup and management of newly diagnosed cirrhosis.
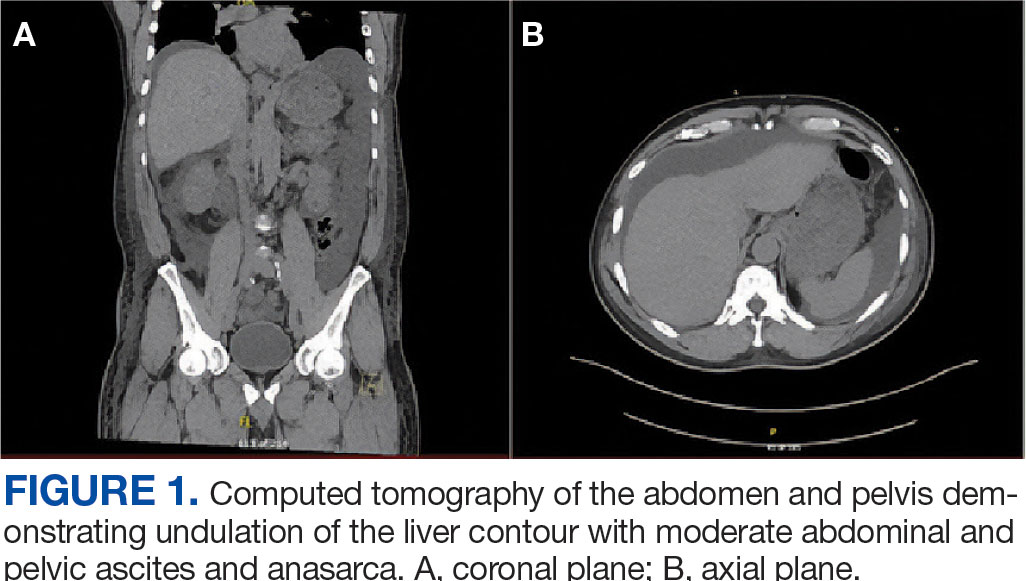
Paracentesis revealed straw-colored fluid with an ascitic fluid neutrophil count of 17/μL, a protein level of < 3 g/dL and albumin level of < 1.5 g/dL. Gram stain of the ascitic fluid showed a moderate white blood cell count with no organisms. Fluid culture showed no microbial growth.
Initial workup for cirrhosis demonstrated a positive total hepatitis A antibody. The patient had a nonreactive hepatitis B surface antigen and surface antibody, but a reactive hepatitis B core antibody; a hepatitis B DNA level was not ordered. He had a reactive hepatitis C antibody with a viral load of 4,490,000 II/mL (genotype 1a). The patient’s iron level was 120 μg/dL, with a calculated total iron-binding capacity (TIBC) of 126.2 μg/dL. His transferrin saturation (TSAT) (serum iron divided by TIBC) was 95%. The patient had nonreactive antinuclear antibody and antimitochondrial antibody tests and a positive antismooth muscle antibody test with a titer of 1:40. His α-fetoprotein (AFP) level was 505 ng/mL (reference range, < 8 ng/mL).
Follow-up MRI of the abdomen and pelvis showed cirrhotic morphology with large volume ascites and portosystemic collaterals, consistent with portal hypertension. Additionally, it showed multiple scattered peripheral sub centimeter hyperenhancing foci, most likely representing benign lesions.
The patient's spot urine protein-creatinine ratio was 3.76. To better quantify proteinuria, a 24-hour urine collection was performed and revealed 12.8 g/d of urine protein (reference range, 0-0.17 g/d). His serum triglyceride level was 175 mg/dL (reference range, 40-60 mg/dL); total cholesterol was 177 mg/ dL (reference range, ≤ 200 mg/dL); low density lipoprotein cholesterol was 98 mg/ dL (reference range, ≤ 130 mg/dL); and highdensity lipoprotein cholesterol was 43.8 mg/ dL (reference range, ≥ 40 mg/dL); C3 complement level was 71 mg/dL (reference range, 82-185 mg/dL); and C4 complement level was 22 mg/dL (reference range, 15-53 mg/ dL). His rheumatoid factor was < 14 IU/mL. Tests for rapid plasma reagin and HIV antigen- antibody were nonreactive, and the phospholipase A2 receptor antibody test was negative. The patient tested positive for QuantiFERON-TB Gold and qualitative cryoglobulin, which indicated a cryocrit of 1%.
A renal biopsy was performed, revealing diffuse podocyte foot process effacement and glomerulonephritis with low-grade C3 and immunoglobulin (Ig) G deposits, consistent with early membranoproliferative glomerulonephritis (MPGN) (Figures 2 and 3).
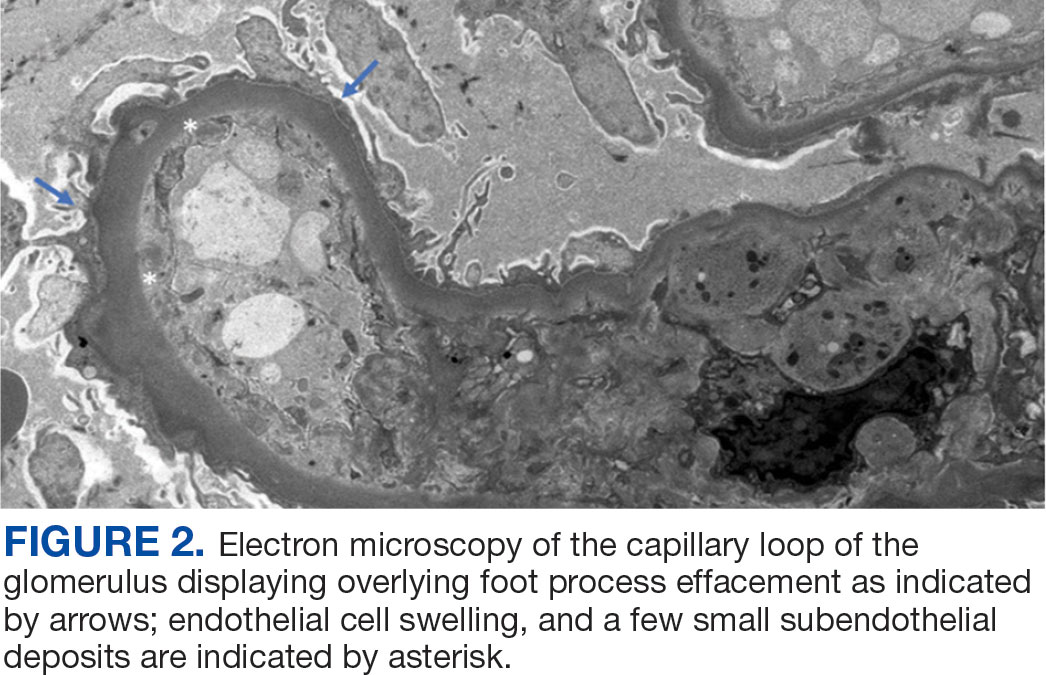
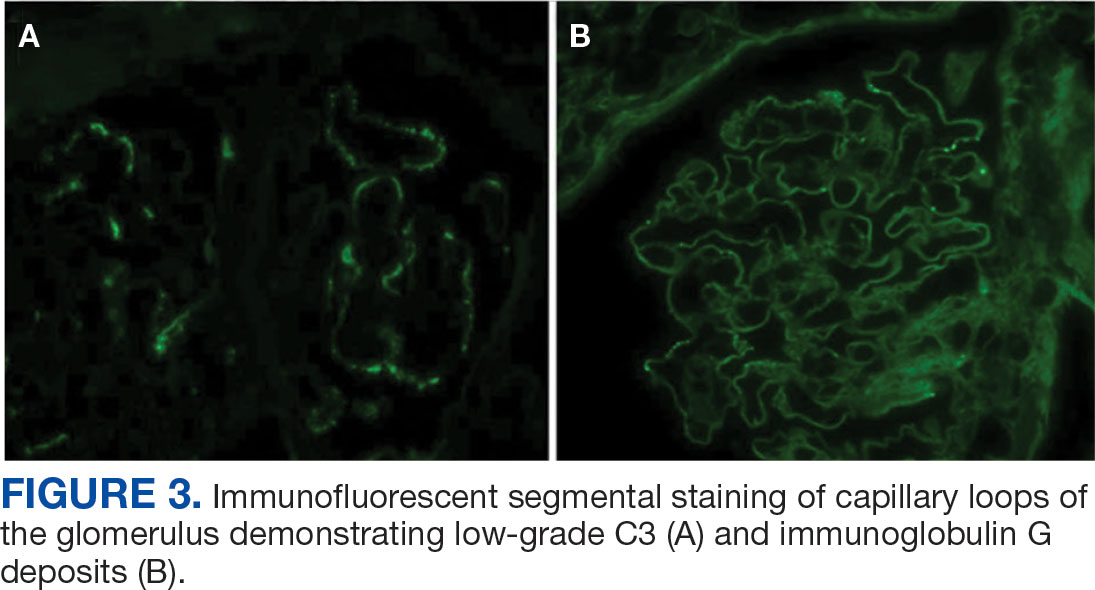
The patient was initially diuresed with IV furosemide without significant urine output. He was then diuresed with IV 25% albumin (total, 25 g), followed by IV furosemide 40 mg twice daily, which led to significant urine output and resolution of his anasarca. Given the patient’s hypoalbuminemic state, IV albumin was necessary to deliver furosemide to the proximal tubule. He was started on lisinopril for renal protection and discharged with spironolactone and furosemide for fluid management in the context of cirrhosis.
The patient was evaluated by the Liver Nodule Clinic, which includes specialists from hepatology, medical oncology, radiation oncology, interventional radiology, and diagnostic radiology. The team considered the patient’s medical history and characteristics of the nodules on imaging. Notable aspects of the patient’s history included hepatitis C virus (HCV) infection and an elevated AFP level, although imaging showed no lesion concerning for malignancy. Given these findings, the patient was scheduled for a liver biopsy to establish a tissue diagnosis of cirrhosis. Hepatology, nephrology, and infectious disease specialists coordinated to plan the management and treatment of latent tuberculosis (TB), chronic HCV, MPGN, compensated cirrhosis, and suspicious liver lesions.
The patient chose to handle management and treatment as an outpatient. He was discharged with furosemide and spironolactone for anasarca management, and amlodipine and lisinopril for his hypertension and MPGN. Follow-up appointments were scheduled with infectious disease for management of latent TB and HCV, nephrology for MPGN, gastroenterology for cirrhosis, and interventional radiology for liver biopsy. Unfortunately, the patient was unhoused with limited access to transportation, which prevented timely follow-up. Given these social factors, immunosuppression was not started. Additionally, he did not start on HCV therapy because the viral load was still pending at time of discharge.
DISCUSSION
The diagnosis of decompensated cirrhosis was prematurely established, resulting in a diagnostic delay, a form of diagnostic error. However, on hospital day 2, the initial hypothesis of decompensated cirrhosis as the sole driver of the patient’s presentation was reconsidered due to the disconnect between the severity of hypoalbuminemia and diffuse edema (anasarca), and the absence of laboratory evidence of hepatic decompensation (normal international normalized ratio, bilirubin, and low but normal platelet count). Although image findings supported cirrhosis, laboratory markers did not indicate hepatic decompensation. The severity of hypoalbuminemia and anasarca, along with an indeterminate Serum-Ascites Albumin Gradient, prompted the patient’s care team to consider other causes, specifically, nephrotic syndrome.
The patien’s spot protein-to-creatinine ratio was 3.76 (reference range < 0.2 mg/mg creatinine), but a 24-hour urine protein collection was 12.8 g/day (reference range < 150 mg/day). While most spot urine protein- to-creatinine ratios (UPCR) correlate with a 24-hour urine collection, discrepancies can occur, as in this case. It is important to recognize that the spot UPCR assumes that patients are excreting 1000 mg of creatinine daily in their urine, which is not always the case. In addition, changes in urine osmolality can lead to different values. The gold standard for proteinuria is a 24-hour urine collection for protein and creatinine.
The patient’s nephrotic-range proteinuria and severe hypoalbuminemia are not solely explained by cirrhosis. In addition, the patient’s lower extremity edema pointed to nephrotic syndrome. The differential diagnosis for nephrotic syndrome includes both primary and secondary forms of membranous nephropathy, minimal change disease, focal segmental glomerulosclerosis, and MPGN, a histopathological diagnosis that requires distinguishing between immune complex-mediated and complement-mediated forms. Other causes of nephrotic syndrome that do not fit in any of these buckets include amyloidosis, IgA nephropathy, and diabetes mellitus (DM). Despite DM being a common cause of nephrotic range proteinuria, it rarely leads to full nephrotic syndrome.
When considering the diagnosis, we reframed the patient’s clinical syndrome as compensated cirrhosis plus nephrotic syndrome. This approach prioritized identifying a cause that could explain both cirrhosis (from any cause) leading to IgA nephropathy or injection drug use serving as a risk factor for cirrhosis and nephrotic syndrome through HCV or AA amyloidosis, respectively. This problem representation guided us to the correct diagnosis. There are multiple renal diseases associated with HCV infection, including MPGN, membranous nephropathy, focal segmental glomerulosclerosis, and IgA nephropathy.2 MPGN and mixed cryoglobulinemia are the most common. In the past, MPGN was classified as type I, II, and III.
The patient’s urine toxicology revealed recent amphetamine use, which can also lead to acute kidney injury through rhabdomyolysis or acute interstitial nephritis (AIN).3 In the cases of rhabdomyolysis, urinalysis would show positive heme without any red blood cell on microscopic analysis, which was not present in this case. AIN commonly manifests as acute kidney injury, pyuria, and proteinuria but without a decrease in complement levels.4 While the patient’s urine sediment included white blood cell (10/high-power field), the presence of microscopic hematuria, decreased complement levels, and proteinuria in the context of HCV positivity makes MPGN more likely than AIN.
Recently, there has been greater emphasis on using immunofluorescence for kidney biopsies. MPGN is now classified into 2 main categories: MPGN with mesangial immunoglobulins and C3 deposits in the capillary walls, and MPGN with C3 deposits but without Ig.5 MPGN with Ig-complement deposits is seen in autoimmune diseases and infections and is associated with dysproteinemias.
The renal biopsy in this patient was consistent with MPGN with immunofluorescence, a common finding in patients with infection. By synthesizing these data, we concluded that the patient represented a case of chronic HCV infection that led to MPGN with cryoglobulinemia. The normal C4 and negative RF do not suggest cryoglobulinemic crisis. Compensated cirrhosis was seen on imaging, pending liver biopsy.
Treatment
The management of MPGN secondary to HCV infection relies on the treatment of the underlying infection and clearance of viral load. Direct-acting antivirals have been used successfully in the treatment of HCV-associated MPGN. When cryoglobulinemia is present, immunosuppressive therapy is recommended. These regimens commonly include rituximab and steroids.5 Rituximab is also used for nephrotic syndrome associated with MPGN, as recommended in the 2018 Kidney Disease: Improving Global Outcomes guidelines.6
When initiating rituximab therapy in a patient who tests positive for hepatitis B (HBcAb positive or HBsAb positive), it is recommended to follow the established guidelines, which include treating them with entecavir for prophylaxis to prevent reactivation or a flare of hepatitis B.7 The patient in this case needed close follow-up in the nephrology and hepatology clinic. Immunosuppressive therapy was not pursued while the patient was admitted to the hospital due to instability with housing, transportation, and difficulty in ensuring close follow-up.
CONCLUSIONS
Clinicians should maintain a broad differential even in the face of confirmatory imaging and other objective findings. In the case of anasarca, nephrotic syndrome should be considered. Key causes of nephrotic syndromes include MPGN, membranous nephropathy, minimal change disease, and focal segmental glomerulosclerosis. MPGN is a histopathological diagnosis, and it is essential to identify if it is secondary to immune complexes or only complement mediated because Ig-complement deposits are seen in autoimmune disease and infection. The management of MPGN due to HCV infection relies on antiviral therapy. In the presence of cryoglobulinemia, immunosuppressive therapy is recommended.
- Tapper EB, Parikh ND. Diagnosis and management of cirrhosis and its complications: a review. JAMA. 2023;329(18):1589–1602. doi:10.1001/jama.2023.5997
- Ozkok A, Yildiz A. Hepatitis C virus associated glomerulopathies. World J Gastroenterol. 2014;20(24):7544-7554. doi:10.3748/wjg.v20.i24.7544
- Foley RJ, Kapatkin K, Vrani R, Weinman EJ. Amphetamineinduced acute renal failure. South Med J. 1984;77(2):258- 260. doi:10.1097/00007611-198402000-00035
- Rossert J. Drug - induced acute interstitial nephritis. Kidney Int. 2001;60(2):804-817. doi:10.1046/j.1523-1755.2001.060002804.x
- Sethi S, Fervenza FC. Membranoproliferative glomerulonephritis: pathogenetic heterogeneity and proposal for a new classification. Semin Nephrol. 2011;31(4):341-348. doi:10.1016/j.semnephrol.2011.06.005
- Jadoul M, Berenguer MC, Doss W, et al. Executive summary of the 2018 KDIGO hepatitis C in CKD guideline: welcoming advances in evaluation and management. Kidney Int. 2018;94(4):663-673. doi:10.1016/j.kint.2018.06.011
- Myint A, Tong MJ, Beaven SW. Reactivation of hepatitis b virus: a review of clinical guidelines. Clin Liver Dis (Hoboken). 2020;15(4):162-167. doi:10.1002/cld.883
- Tapper EB, Parikh ND. Diagnosis and management of cirrhosis and its complications: a review. JAMA. 2023;329(18):1589–1602. doi:10.1001/jama.2023.5997
- Ozkok A, Yildiz A. Hepatitis C virus associated glomerulopathies. World J Gastroenterol. 2014;20(24):7544-7554. doi:10.3748/wjg.v20.i24.7544
- Foley RJ, Kapatkin K, Vrani R, Weinman EJ. Amphetamineinduced acute renal failure. South Med J. 1984;77(2):258- 260. doi:10.1097/00007611-198402000-00035
- Rossert J. Drug - induced acute interstitial nephritis. Kidney Int. 2001;60(2):804-817. doi:10.1046/j.1523-1755.2001.060002804.x
- Sethi S, Fervenza FC. Membranoproliferative glomerulonephritis: pathogenetic heterogeneity and proposal for a new classification. Semin Nephrol. 2011;31(4):341-348. doi:10.1016/j.semnephrol.2011.06.005
- Jadoul M, Berenguer MC, Doss W, et al. Executive summary of the 2018 KDIGO hepatitis C in CKD guideline: welcoming advances in evaluation and management. Kidney Int. 2018;94(4):663-673. doi:10.1016/j.kint.2018.06.011
- Myint A, Tong MJ, Beaven SW. Reactivation of hepatitis b virus: a review of clinical guidelines. Clin Liver Dis (Hoboken). 2020;15(4):162-167. doi:10.1002/cld.883
Elusive Edema: A Case of Nephrotic Syndrome Mimicking Decompensated Cirrhosis
Elusive Edema: A Case of Nephrotic Syndrome Mimicking Decompensated Cirrhosis
Intensive BP Control May Benefit CKD Patients in Real World
TOPLINE:
The cardiovascular benefits observed with intensive blood pressure (BP) control in patients with hypertension and elevated cardiovascular risk from the Systolic Blood Pressure Intervention Trial (SPRINT) can be largely replicated in real-world settings among patients with chronic kidney disease (CKD), highlighting the advantages of adopting intensive BP targets.
METHODOLOGY:
- Researchers conducted a comparative effectiveness study to determine if the beneficial and adverse effects of intensive vs standard BP control observed in SPRINT were replicable in patients with CKD and hypertension in clinical practice.
- They identified 85,938 patients (mean age, 75.7 years; 95.0% men) and 13,983 patients (mean age, 77.4 years; 38.4% men) from the Veterans Health Administration (VHA) and Kaiser Permanente of Southern California (KPSC) databases, respectively.
- The treatment effect was estimated by combining baseline covariate, treatment, and outcome data of participants from the SPRINT with covariate data from the VHA and KPSC databases.
- The primary outcomes included major cardiovascular events, all-cause death, cognitive impairment, CKD progression, and adverse events at 4 years.
TAKEAWAY:
- Compared with SPRINT participants, those in the VHA and KPSC databases were older, had less prevalent cardiovascular disease, higher albuminuria, and used more statins.
- The benefits of intensive vs standard BP control on major cardiovascular events, all-cause mortality, and certain adverse events (hypotension, syncope, bradycardia, acute kidney injury, and electrolyte abnormality) were transferable from the trial to the VHA and KPSC populations.
- The treatment effect of intensive BP management on CKD progression was transportable to the KPSC population but not to the VHA population. However, the trial’s impact on cognitive outcomes, such as dementia, was not transportable to either the VHA or KPSC populations.
- On the absolute scale, intensive vs standard BP treatment showed greater cardiovascular benefits and fewer safety concerns in the VHA and KPSC populations than in the SPRINT.
IN PRACTICE:
“This example highlights the potential for transportability methods to provide insights that can bridge evidence gaps and inform the application of novel therapies to patients with CKD who are treated in everyday practice,” the authors wrote.
SOURCE:
This study was led by Manjula Kurella Tamura, MD, MPH, Division of Nephrology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California. It was published online on January 7, 2025, in JAMA Network Open.
LIMITATIONS:
Transportability analyses could not account for characteristics that were not well-documented in electronic health records, such as limited life expectancy. The study was conducted before the widespread use of sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and nonsteroidal mineralocorticoid receptor antagonists, making it unclear whether intensive BP treatment would result in similar benefits with current pharmacotherapy regimens. Eligibility for this study was based on BP measurements in routine practice, which tend to be more variable than those collected in research settings.
DISCLOSURES:
This study was supported by grants from the National Institutes of Health. Some authors disclosed serving as a consultant and receiving grants, personal fees, and consulting fees from pharmaceutical companies and other sources.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The cardiovascular benefits observed with intensive blood pressure (BP) control in patients with hypertension and elevated cardiovascular risk from the Systolic Blood Pressure Intervention Trial (SPRINT) can be largely replicated in real-world settings among patients with chronic kidney disease (CKD), highlighting the advantages of adopting intensive BP targets.
METHODOLOGY:
- Researchers conducted a comparative effectiveness study to determine if the beneficial and adverse effects of intensive vs standard BP control observed in SPRINT were replicable in patients with CKD and hypertension in clinical practice.
- They identified 85,938 patients (mean age, 75.7 years; 95.0% men) and 13,983 patients (mean age, 77.4 years; 38.4% men) from the Veterans Health Administration (VHA) and Kaiser Permanente of Southern California (KPSC) databases, respectively.
- The treatment effect was estimated by combining baseline covariate, treatment, and outcome data of participants from the SPRINT with covariate data from the VHA and KPSC databases.
- The primary outcomes included major cardiovascular events, all-cause death, cognitive impairment, CKD progression, and adverse events at 4 years.
TAKEAWAY:
- Compared with SPRINT participants, those in the VHA and KPSC databases were older, had less prevalent cardiovascular disease, higher albuminuria, and used more statins.
- The benefits of intensive vs standard BP control on major cardiovascular events, all-cause mortality, and certain adverse events (hypotension, syncope, bradycardia, acute kidney injury, and electrolyte abnormality) were transferable from the trial to the VHA and KPSC populations.
- The treatment effect of intensive BP management on CKD progression was transportable to the KPSC population but not to the VHA population. However, the trial’s impact on cognitive outcomes, such as dementia, was not transportable to either the VHA or KPSC populations.
- On the absolute scale, intensive vs standard BP treatment showed greater cardiovascular benefits and fewer safety concerns in the VHA and KPSC populations than in the SPRINT.
IN PRACTICE:
“This example highlights the potential for transportability methods to provide insights that can bridge evidence gaps and inform the application of novel therapies to patients with CKD who are treated in everyday practice,” the authors wrote.
SOURCE:
This study was led by Manjula Kurella Tamura, MD, MPH, Division of Nephrology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California. It was published online on January 7, 2025, in JAMA Network Open.
LIMITATIONS:
Transportability analyses could not account for characteristics that were not well-documented in electronic health records, such as limited life expectancy. The study was conducted before the widespread use of sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and nonsteroidal mineralocorticoid receptor antagonists, making it unclear whether intensive BP treatment would result in similar benefits with current pharmacotherapy regimens. Eligibility for this study was based on BP measurements in routine practice, which tend to be more variable than those collected in research settings.
DISCLOSURES:
This study was supported by grants from the National Institutes of Health. Some authors disclosed serving as a consultant and receiving grants, personal fees, and consulting fees from pharmaceutical companies and other sources.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The cardiovascular benefits observed with intensive blood pressure (BP) control in patients with hypertension and elevated cardiovascular risk from the Systolic Blood Pressure Intervention Trial (SPRINT) can be largely replicated in real-world settings among patients with chronic kidney disease (CKD), highlighting the advantages of adopting intensive BP targets.
METHODOLOGY:
- Researchers conducted a comparative effectiveness study to determine if the beneficial and adverse effects of intensive vs standard BP control observed in SPRINT were replicable in patients with CKD and hypertension in clinical practice.
- They identified 85,938 patients (mean age, 75.7 years; 95.0% men) and 13,983 patients (mean age, 77.4 years; 38.4% men) from the Veterans Health Administration (VHA) and Kaiser Permanente of Southern California (KPSC) databases, respectively.
- The treatment effect was estimated by combining baseline covariate, treatment, and outcome data of participants from the SPRINT with covariate data from the VHA and KPSC databases.
- The primary outcomes included major cardiovascular events, all-cause death, cognitive impairment, CKD progression, and adverse events at 4 years.
TAKEAWAY:
- Compared with SPRINT participants, those in the VHA and KPSC databases were older, had less prevalent cardiovascular disease, higher albuminuria, and used more statins.
- The benefits of intensive vs standard BP control on major cardiovascular events, all-cause mortality, and certain adverse events (hypotension, syncope, bradycardia, acute kidney injury, and electrolyte abnormality) were transferable from the trial to the VHA and KPSC populations.
- The treatment effect of intensive BP management on CKD progression was transportable to the KPSC population but not to the VHA population. However, the trial’s impact on cognitive outcomes, such as dementia, was not transportable to either the VHA or KPSC populations.
- On the absolute scale, intensive vs standard BP treatment showed greater cardiovascular benefits and fewer safety concerns in the VHA and KPSC populations than in the SPRINT.
IN PRACTICE:
“This example highlights the potential for transportability methods to provide insights that can bridge evidence gaps and inform the application of novel therapies to patients with CKD who are treated in everyday practice,” the authors wrote.
SOURCE:
This study was led by Manjula Kurella Tamura, MD, MPH, Division of Nephrology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California. It was published online on January 7, 2025, in JAMA Network Open.
LIMITATIONS:
Transportability analyses could not account for characteristics that were not well-documented in electronic health records, such as limited life expectancy. The study was conducted before the widespread use of sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and nonsteroidal mineralocorticoid receptor antagonists, making it unclear whether intensive BP treatment would result in similar benefits with current pharmacotherapy regimens. Eligibility for this study was based on BP measurements in routine practice, which tend to be more variable than those collected in research settings.
DISCLOSURES:
This study was supported by grants from the National Institutes of Health. Some authors disclosed serving as a consultant and receiving grants, personal fees, and consulting fees from pharmaceutical companies and other sources.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Lowering Urate May Protect Kidneys in Gout Patients With CKD
TOPLINE:
Achieving serum urate to below 6 mg/dL with urate-lowering therapy (ULT) in patients with gout and chronic kidney disease (CKD) stage III is not linked to an increased risk for severe or end-stage kidney disease.
METHODOLOGY:
- Researchers emulated analyses of a hypothetical target trial using a cloning, censoring, and weighting approach to evaluate the association between achieving target serum urate level with ULT and the progression of CKD in patients with gout and CKD stage III.
- They included 14,972 patients (mean age, 73.1 years; 37.7% women) from a general practice database who had a mean baseline serum urate level of 8.9 mg/dL and initiated ULTs such as allopurinol or febuxostat.
- Participants were divided into two groups: Those who achieved a target serum urate level < 6 mg/dL and those who did not within 1 year after the initiation of ULT; the mean follow-up duration was a little more than 3 years in both groups.
- The primary outcome was the occurrence of severe or end-stage kidney disease over 5 years of initiating ULT, defined by an estimated glomerular filtration rate below 30 mL/min per 1.73 m2 on two occasions more than 90 days apart within 1 year, or at least one Read code for CKD stages IV or V, dialysis, or kidney transplant.
- A prespecified noninferiority margin for the hazard ratio was set at 1.2 to compare the outcomes between those who achieved the target serum urate level < 6 mg/dL and those who did not.
TAKEAWAY:
- Among the patients who initiated ULT, 31.8% achieved a target serum urate level < 6 mg/dL within 1 year.
- The 5-year risk for severe or end-stage kidney disease was lower (10.32%) in participants with gout and stage III CKD who achieved the target serum urate level than in those who did not (12.73%).
- The adjusted 5-year risk difference for severe to end-stage kidney disease was not inferior in patients who achieved the target serum urate level vs those who did not (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.80-0.98; P for noninferiority < .001); results were consistent for end-stage kidney disease alone (aHR, 0.67; P for noninferiority = .001).
- Similarly, in participants with gout and CKD stages II-III, the 5-year risks for severe or end-stage kidney disease (aHR, 0.91) and end-stage kidney disease alone (aHR, 0.73) were noninferior in the group that did vs that did not achieve target serum urate levels, with P for noninferiority being < .001 and .003, respectively.
IN PRACTICE:
“Our findings suggest that lowering serum urate levels to < 6 mg/dL is generally well tolerated and may even slow CKD progression in these individuals. Initiatives to optimize the use and adherence to ULT could benefit clinicians and patients,” the authors wrote.
SOURCE:
This study was led by Yilun Wang, MD, PhD, Xiangya Hospital, Central South University, Changsha, China. It was published online in JAMA Internal Medicine.
LIMITATIONS:
Residual confounding may still have been present despite rigorous methods to control it, as is common in observational studies. Participants who achieved target serum urate levels may have received better healthcare, adhered to other treatments more consistently, and used ULT for a longer duration. The findings may have limited generalizability, as participants who did not achieve target serum urate levels prior to initiation were excluded.
DISCLOSURES:
This study was supported by the China National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of the National Clinical Research Center for Geriatric Disorders, and other sources. Two authors reported receiving personal fees and/or grants from multiple pharmaceutical companies.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Achieving serum urate to below 6 mg/dL with urate-lowering therapy (ULT) in patients with gout and chronic kidney disease (CKD) stage III is not linked to an increased risk for severe or end-stage kidney disease.
METHODOLOGY:
- Researchers emulated analyses of a hypothetical target trial using a cloning, censoring, and weighting approach to evaluate the association between achieving target serum urate level with ULT and the progression of CKD in patients with gout and CKD stage III.
- They included 14,972 patients (mean age, 73.1 years; 37.7% women) from a general practice database who had a mean baseline serum urate level of 8.9 mg/dL and initiated ULTs such as allopurinol or febuxostat.
- Participants were divided into two groups: Those who achieved a target serum urate level < 6 mg/dL and those who did not within 1 year after the initiation of ULT; the mean follow-up duration was a little more than 3 years in both groups.
- The primary outcome was the occurrence of severe or end-stage kidney disease over 5 years of initiating ULT, defined by an estimated glomerular filtration rate below 30 mL/min per 1.73 m2 on two occasions more than 90 days apart within 1 year, or at least one Read code for CKD stages IV or V, dialysis, or kidney transplant.
- A prespecified noninferiority margin for the hazard ratio was set at 1.2 to compare the outcomes between those who achieved the target serum urate level < 6 mg/dL and those who did not.
TAKEAWAY:
- Among the patients who initiated ULT, 31.8% achieved a target serum urate level < 6 mg/dL within 1 year.
- The 5-year risk for severe or end-stage kidney disease was lower (10.32%) in participants with gout and stage III CKD who achieved the target serum urate level than in those who did not (12.73%).
- The adjusted 5-year risk difference for severe to end-stage kidney disease was not inferior in patients who achieved the target serum urate level vs those who did not (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.80-0.98; P for noninferiority < .001); results were consistent for end-stage kidney disease alone (aHR, 0.67; P for noninferiority = .001).
- Similarly, in participants with gout and CKD stages II-III, the 5-year risks for severe or end-stage kidney disease (aHR, 0.91) and end-stage kidney disease alone (aHR, 0.73) were noninferior in the group that did vs that did not achieve target serum urate levels, with P for noninferiority being < .001 and .003, respectively.
IN PRACTICE:
“Our findings suggest that lowering serum urate levels to < 6 mg/dL is generally well tolerated and may even slow CKD progression in these individuals. Initiatives to optimize the use and adherence to ULT could benefit clinicians and patients,” the authors wrote.
SOURCE:
This study was led by Yilun Wang, MD, PhD, Xiangya Hospital, Central South University, Changsha, China. It was published online in JAMA Internal Medicine.
LIMITATIONS:
Residual confounding may still have been present despite rigorous methods to control it, as is common in observational studies. Participants who achieved target serum urate levels may have received better healthcare, adhered to other treatments more consistently, and used ULT for a longer duration. The findings may have limited generalizability, as participants who did not achieve target serum urate levels prior to initiation were excluded.
DISCLOSURES:
This study was supported by the China National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of the National Clinical Research Center for Geriatric Disorders, and other sources. Two authors reported receiving personal fees and/or grants from multiple pharmaceutical companies.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Achieving serum urate to below 6 mg/dL with urate-lowering therapy (ULT) in patients with gout and chronic kidney disease (CKD) stage III is not linked to an increased risk for severe or end-stage kidney disease.
METHODOLOGY:
- Researchers emulated analyses of a hypothetical target trial using a cloning, censoring, and weighting approach to evaluate the association between achieving target serum urate level with ULT and the progression of CKD in patients with gout and CKD stage III.
- They included 14,972 patients (mean age, 73.1 years; 37.7% women) from a general practice database who had a mean baseline serum urate level of 8.9 mg/dL and initiated ULTs such as allopurinol or febuxostat.
- Participants were divided into two groups: Those who achieved a target serum urate level < 6 mg/dL and those who did not within 1 year after the initiation of ULT; the mean follow-up duration was a little more than 3 years in both groups.
- The primary outcome was the occurrence of severe or end-stage kidney disease over 5 years of initiating ULT, defined by an estimated glomerular filtration rate below 30 mL/min per 1.73 m2 on two occasions more than 90 days apart within 1 year, or at least one Read code for CKD stages IV or V, dialysis, or kidney transplant.
- A prespecified noninferiority margin for the hazard ratio was set at 1.2 to compare the outcomes between those who achieved the target serum urate level < 6 mg/dL and those who did not.
TAKEAWAY:
- Among the patients who initiated ULT, 31.8% achieved a target serum urate level < 6 mg/dL within 1 year.
- The 5-year risk for severe or end-stage kidney disease was lower (10.32%) in participants with gout and stage III CKD who achieved the target serum urate level than in those who did not (12.73%).
- The adjusted 5-year risk difference for severe to end-stage kidney disease was not inferior in patients who achieved the target serum urate level vs those who did not (adjusted hazard ratio [aHR], 0.89; 95% CI, 0.80-0.98; P for noninferiority < .001); results were consistent for end-stage kidney disease alone (aHR, 0.67; P for noninferiority = .001).
- Similarly, in participants with gout and CKD stages II-III, the 5-year risks for severe or end-stage kidney disease (aHR, 0.91) and end-stage kidney disease alone (aHR, 0.73) were noninferior in the group that did vs that did not achieve target serum urate levels, with P for noninferiority being < .001 and .003, respectively.
IN PRACTICE:
“Our findings suggest that lowering serum urate levels to < 6 mg/dL is generally well tolerated and may even slow CKD progression in these individuals. Initiatives to optimize the use and adherence to ULT could benefit clinicians and patients,” the authors wrote.
SOURCE:
This study was led by Yilun Wang, MD, PhD, Xiangya Hospital, Central South University, Changsha, China. It was published online in JAMA Internal Medicine.
LIMITATIONS:
Residual confounding may still have been present despite rigorous methods to control it, as is common in observational studies. Participants who achieved target serum urate levels may have received better healthcare, adhered to other treatments more consistently, and used ULT for a longer duration. The findings may have limited generalizability, as participants who did not achieve target serum urate levels prior to initiation were excluded.
DISCLOSURES:
This study was supported by the China National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of the National Clinical Research Center for Geriatric Disorders, and other sources. Two authors reported receiving personal fees and/or grants from multiple pharmaceutical companies.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
How to Avoid Freaking Out About Kidney Function
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr Paul Nelson Williams.
We had a great discussion with Kidney Boy, Dr Joel Topf, everyone’s favorite nephrologist, and he taught us how to manage blood pressure in chronic kidney disease (CKD).
Paul N. Williams, MD: Dr Topf focuses more on albuminuria than we are used to doing. It’s probably one of the most important prognostic indicators of how a patient is going to do from a renal standpoint.
Historically, I’ve tended to focus on the estimated glomerular filtration rate (eGFR), and the lower that number gets, the more I sweat, but albuminuria is probably equally, if not more, important as a way of prognosticating whether a patient is going to progress to dialysis or transplant. He directed us towards this nifty little calculator, kidneyfailurerisk.com, where you plug in the patient’s age, eGFR, and degree of albuminuria, and it spits out their risk of progressing to hemodialysis or renal transplantation over the next 5 years. It’s a nice way to concretely explain to patients their risk for progression.
Instead of telling the patient, “You are high risk,” Dr Topf will say, “Your risk is 6% of needing dialysis in the next 5 years.” You can even use these thresholds to gauge when to refer a patient. If someone has a 5-year risk between 3% and 5% or higher, that patient should probably be seeing a nephrologist.
If their 2-year risk is greater than 20%, that patient probably should be evaluated for transplantation. This gives us have more concrete numbers to work with rather than just saying, “Your kidneys aren’t working as well as we would like and you should see a kidney doctor.” Patients have a better sense of how serious things might be.
Watto: It’s just easier for them to understand. Dr Topf made the point that we used to have a heat map based on the stage of CKD that would tell you how high a patient’s risk was compared with other people. But patients don’t really understand relative risk, so Dr Topf tells them their absolute risk for ending up on dialysis over the next 2-5 years.
Patients come in and they are worried because they looked at their lab results and see that their creatinine level is red, or their eGFR is low. They think, It says I have stage 3a CKD.
We should probably have the stages of CKD start at stage 3, which should be called stage 1 so it doesn’t sound as bad. Patients think they are halfway to dialysis; they are already at stage 3 and didn’t even know their kidneys were a problem.
Dr Topf said that cystatin C (something I only recently started ordering) can be obtained, and sometimes you can recategorize the patient, especially those with an eGFR between 45 and 60. The cystatin C can predict their renal function better than the creatinine-based equations. If you are using the creatinine equation, he recommends using the 2021 equations.
Another nice thing about cystatin C is that it isn’t tripped up in younger patients with a lot of muscle mass. You just have to watch out for inflammation, which can throw the test off. For example, when a patient is in the intensive care unit, it’s probably not that helpful, but for your outpatients, cystatin C works well.
Williams: I’ve been using it a fair amount in my patients with more muscle mass. And some patients have been taking creatine as a supplement, and that can alter the numbers as well. This is a nice way to get them out of CKD stage 2 or 3 and back where they belong, with normal healthy functioning kidneys.
Watto: Now, Paul, if we find a patient with more advanced CKD — let’s say stage 4, whether by cystatin C or serum creatinine, and their eGFR is less than 30 — should we start peeling off the angiotensin-converting enzyme ACE inhibitor or the angiotensin receptor blocker (ARB)? Those drugs can raise potassium. What should we do here?
Williams: That’s the temptation, Matt, and I feel like that was the old orthodoxy, back in residency. It didn’t take much for us to start taking off ACE inhibitors or ARBs once the kidney function started to drop, but it turns out you may be doing more harm than good.
Some data have shown that if you peel off those medications, you actually increase mortality and cardiovascular risk. So, in general, if you can keep them going, the patient will be better off. Hang onto the ACE inhibitors or ARBs as long as you are able to, because they confer a fair amount of benefit.
Watto: As long as the potassium isn’t in red on your lab’s range. It might go up to 5.2 or 5.4, but as long as it’s stable, that should be OK. You probably wouldn’t initiate an ACE inhibitor or ARB or spironolactone with a potassium level above 5, but if it’s below 5 when you start and it goes up slightly after you start the drug, that could be acceptable.
Another thing we talked about was when a patient progresses to CKD and ends up on dialysis, how helpful are those intradialysis blood pressures in predicting cardiovascular outcomes?
Williams: For someone who’s performing the dialysis, probably really helpful. In the outpatient setting to predict cardiovascular risk, probably less so. Dr Topf makes the point that the readings are done either shortly after or right when the patient is about to have a large-bore catheter inserted into their arm. And then they have liters of fluid drained out of them. So those numbers are going to have huge amounts of variability. You would not base the patient’s blood pressure treatment solely on those numbers. But regardless of what the numbers are, or even regardless of your office numbers, hopefully you’re working with a nephrologist to make sure that you’re actually in concert and not fighting each other with the blood pressure medications.
Watto: Dr Topf said that a lot of the hypertension in dialysis is because of too much volume. If you can get the volume down, you might be able to peel off blood pressure medications instead of adding more. But some patients have issues with cramping; it’s uncomfortable and not everyone tolerates it.
I was really surprised to learn that beta blockers, specifically atenolol, have some evidence of improving cardiovascular outcomes in patients on dialysis. Dr Topf speculated that this was because they are largely dying of cardiovascular disease, so maybe that’s why, but that’s one of the places, the only places I can think of aside from thyroid disease, where atenolol really shines.
If you want to hear this fantastic episode and all the great pearls, then click on this link.
Matthew F. Watto, MD, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, disclosed no relevant financial relationships. Paul N. Williams, MD, has disclosed ties with The Curbsiders.
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr Paul Nelson Williams.
We had a great discussion with Kidney Boy, Dr Joel Topf, everyone’s favorite nephrologist, and he taught us how to manage blood pressure in chronic kidney disease (CKD).
Paul N. Williams, MD: Dr Topf focuses more on albuminuria than we are used to doing. It’s probably one of the most important prognostic indicators of how a patient is going to do from a renal standpoint.
Historically, I’ve tended to focus on the estimated glomerular filtration rate (eGFR), and the lower that number gets, the more I sweat, but albuminuria is probably equally, if not more, important as a way of prognosticating whether a patient is going to progress to dialysis or transplant. He directed us towards this nifty little calculator, kidneyfailurerisk.com, where you plug in the patient’s age, eGFR, and degree of albuminuria, and it spits out their risk of progressing to hemodialysis or renal transplantation over the next 5 years. It’s a nice way to concretely explain to patients their risk for progression.
Instead of telling the patient, “You are high risk,” Dr Topf will say, “Your risk is 6% of needing dialysis in the next 5 years.” You can even use these thresholds to gauge when to refer a patient. If someone has a 5-year risk between 3% and 5% or higher, that patient should probably be seeing a nephrologist.
If their 2-year risk is greater than 20%, that patient probably should be evaluated for transplantation. This gives us have more concrete numbers to work with rather than just saying, “Your kidneys aren’t working as well as we would like and you should see a kidney doctor.” Patients have a better sense of how serious things might be.
Watto: It’s just easier for them to understand. Dr Topf made the point that we used to have a heat map based on the stage of CKD that would tell you how high a patient’s risk was compared with other people. But patients don’t really understand relative risk, so Dr Topf tells them their absolute risk for ending up on dialysis over the next 2-5 years.
Patients come in and they are worried because they looked at their lab results and see that their creatinine level is red, or their eGFR is low. They think, It says I have stage 3a CKD.
We should probably have the stages of CKD start at stage 3, which should be called stage 1 so it doesn’t sound as bad. Patients think they are halfway to dialysis; they are already at stage 3 and didn’t even know their kidneys were a problem.
Dr Topf said that cystatin C (something I only recently started ordering) can be obtained, and sometimes you can recategorize the patient, especially those with an eGFR between 45 and 60. The cystatin C can predict their renal function better than the creatinine-based equations. If you are using the creatinine equation, he recommends using the 2021 equations.
Another nice thing about cystatin C is that it isn’t tripped up in younger patients with a lot of muscle mass. You just have to watch out for inflammation, which can throw the test off. For example, when a patient is in the intensive care unit, it’s probably not that helpful, but for your outpatients, cystatin C works well.
Williams: I’ve been using it a fair amount in my patients with more muscle mass. And some patients have been taking creatine as a supplement, and that can alter the numbers as well. This is a nice way to get them out of CKD stage 2 or 3 and back where they belong, with normal healthy functioning kidneys.
Watto: Now, Paul, if we find a patient with more advanced CKD — let’s say stage 4, whether by cystatin C or serum creatinine, and their eGFR is less than 30 — should we start peeling off the angiotensin-converting enzyme ACE inhibitor or the angiotensin receptor blocker (ARB)? Those drugs can raise potassium. What should we do here?
Williams: That’s the temptation, Matt, and I feel like that was the old orthodoxy, back in residency. It didn’t take much for us to start taking off ACE inhibitors or ARBs once the kidney function started to drop, but it turns out you may be doing more harm than good.
Some data have shown that if you peel off those medications, you actually increase mortality and cardiovascular risk. So, in general, if you can keep them going, the patient will be better off. Hang onto the ACE inhibitors or ARBs as long as you are able to, because they confer a fair amount of benefit.
Watto: As long as the potassium isn’t in red on your lab’s range. It might go up to 5.2 or 5.4, but as long as it’s stable, that should be OK. You probably wouldn’t initiate an ACE inhibitor or ARB or spironolactone with a potassium level above 5, but if it’s below 5 when you start and it goes up slightly after you start the drug, that could be acceptable.
Another thing we talked about was when a patient progresses to CKD and ends up on dialysis, how helpful are those intradialysis blood pressures in predicting cardiovascular outcomes?
Williams: For someone who’s performing the dialysis, probably really helpful. In the outpatient setting to predict cardiovascular risk, probably less so. Dr Topf makes the point that the readings are done either shortly after or right when the patient is about to have a large-bore catheter inserted into their arm. And then they have liters of fluid drained out of them. So those numbers are going to have huge amounts of variability. You would not base the patient’s blood pressure treatment solely on those numbers. But regardless of what the numbers are, or even regardless of your office numbers, hopefully you’re working with a nephrologist to make sure that you’re actually in concert and not fighting each other with the blood pressure medications.
Watto: Dr Topf said that a lot of the hypertension in dialysis is because of too much volume. If you can get the volume down, you might be able to peel off blood pressure medications instead of adding more. But some patients have issues with cramping; it’s uncomfortable and not everyone tolerates it.
I was really surprised to learn that beta blockers, specifically atenolol, have some evidence of improving cardiovascular outcomes in patients on dialysis. Dr Topf speculated that this was because they are largely dying of cardiovascular disease, so maybe that’s why, but that’s one of the places, the only places I can think of aside from thyroid disease, where atenolol really shines.
If you want to hear this fantastic episode and all the great pearls, then click on this link.
Matthew F. Watto, MD, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, disclosed no relevant financial relationships. Paul N. Williams, MD, has disclosed ties with The Curbsiders.
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr Paul Nelson Williams.
We had a great discussion with Kidney Boy, Dr Joel Topf, everyone’s favorite nephrologist, and he taught us how to manage blood pressure in chronic kidney disease (CKD).
Paul N. Williams, MD: Dr Topf focuses more on albuminuria than we are used to doing. It’s probably one of the most important prognostic indicators of how a patient is going to do from a renal standpoint.
Historically, I’ve tended to focus on the estimated glomerular filtration rate (eGFR), and the lower that number gets, the more I sweat, but albuminuria is probably equally, if not more, important as a way of prognosticating whether a patient is going to progress to dialysis or transplant. He directed us towards this nifty little calculator, kidneyfailurerisk.com, where you plug in the patient’s age, eGFR, and degree of albuminuria, and it spits out their risk of progressing to hemodialysis or renal transplantation over the next 5 years. It’s a nice way to concretely explain to patients their risk for progression.
Instead of telling the patient, “You are high risk,” Dr Topf will say, “Your risk is 6% of needing dialysis in the next 5 years.” You can even use these thresholds to gauge when to refer a patient. If someone has a 5-year risk between 3% and 5% or higher, that patient should probably be seeing a nephrologist.
If their 2-year risk is greater than 20%, that patient probably should be evaluated for transplantation. This gives us have more concrete numbers to work with rather than just saying, “Your kidneys aren’t working as well as we would like and you should see a kidney doctor.” Patients have a better sense of how serious things might be.
Watto: It’s just easier for them to understand. Dr Topf made the point that we used to have a heat map based on the stage of CKD that would tell you how high a patient’s risk was compared with other people. But patients don’t really understand relative risk, so Dr Topf tells them their absolute risk for ending up on dialysis over the next 2-5 years.
Patients come in and they are worried because they looked at their lab results and see that their creatinine level is red, or their eGFR is low. They think, It says I have stage 3a CKD.
We should probably have the stages of CKD start at stage 3, which should be called stage 1 so it doesn’t sound as bad. Patients think they are halfway to dialysis; they are already at stage 3 and didn’t even know their kidneys were a problem.
Dr Topf said that cystatin C (something I only recently started ordering) can be obtained, and sometimes you can recategorize the patient, especially those with an eGFR between 45 and 60. The cystatin C can predict their renal function better than the creatinine-based equations. If you are using the creatinine equation, he recommends using the 2021 equations.
Another nice thing about cystatin C is that it isn’t tripped up in younger patients with a lot of muscle mass. You just have to watch out for inflammation, which can throw the test off. For example, when a patient is in the intensive care unit, it’s probably not that helpful, but for your outpatients, cystatin C works well.
Williams: I’ve been using it a fair amount in my patients with more muscle mass. And some patients have been taking creatine as a supplement, and that can alter the numbers as well. This is a nice way to get them out of CKD stage 2 or 3 and back where they belong, with normal healthy functioning kidneys.
Watto: Now, Paul, if we find a patient with more advanced CKD — let’s say stage 4, whether by cystatin C or serum creatinine, and their eGFR is less than 30 — should we start peeling off the angiotensin-converting enzyme ACE inhibitor or the angiotensin receptor blocker (ARB)? Those drugs can raise potassium. What should we do here?
Williams: That’s the temptation, Matt, and I feel like that was the old orthodoxy, back in residency. It didn’t take much for us to start taking off ACE inhibitors or ARBs once the kidney function started to drop, but it turns out you may be doing more harm than good.
Some data have shown that if you peel off those medications, you actually increase mortality and cardiovascular risk. So, in general, if you can keep them going, the patient will be better off. Hang onto the ACE inhibitors or ARBs as long as you are able to, because they confer a fair amount of benefit.
Watto: As long as the potassium isn’t in red on your lab’s range. It might go up to 5.2 or 5.4, but as long as it’s stable, that should be OK. You probably wouldn’t initiate an ACE inhibitor or ARB or spironolactone with a potassium level above 5, but if it’s below 5 when you start and it goes up slightly after you start the drug, that could be acceptable.
Another thing we talked about was when a patient progresses to CKD and ends up on dialysis, how helpful are those intradialysis blood pressures in predicting cardiovascular outcomes?
Williams: For someone who’s performing the dialysis, probably really helpful. In the outpatient setting to predict cardiovascular risk, probably less so. Dr Topf makes the point that the readings are done either shortly after or right when the patient is about to have a large-bore catheter inserted into their arm. And then they have liters of fluid drained out of them. So those numbers are going to have huge amounts of variability. You would not base the patient’s blood pressure treatment solely on those numbers. But regardless of what the numbers are, or even regardless of your office numbers, hopefully you’re working with a nephrologist to make sure that you’re actually in concert and not fighting each other with the blood pressure medications.
Watto: Dr Topf said that a lot of the hypertension in dialysis is because of too much volume. If you can get the volume down, you might be able to peel off blood pressure medications instead of adding more. But some patients have issues with cramping; it’s uncomfortable and not everyone tolerates it.
I was really surprised to learn that beta blockers, specifically atenolol, have some evidence of improving cardiovascular outcomes in patients on dialysis. Dr Topf speculated that this was because they are largely dying of cardiovascular disease, so maybe that’s why, but that’s one of the places, the only places I can think of aside from thyroid disease, where atenolol really shines.
If you want to hear this fantastic episode and all the great pearls, then click on this link.
Matthew F. Watto, MD, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, disclosed no relevant financial relationships. Paul N. Williams, MD, has disclosed ties with The Curbsiders.
An 81-Year-Old White Woman Presented With a 2-Week History of a Painful Lesion on Her Left Calf
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare condition most commonly observed in patients with end-stage renal disease (ESRD). Because of the non-healing nature of the wounds and need for frequent hospitalizations, there is a significant risk of sepsis with a 1-year mortality rate greater than 50%.
Beyond ESRD, calciphylaxis is also associated with obesity, diabetes, hypoalbuminemia, autoimmune conditions, hepatic disease, malignancies, and dialysis. Rates in patients on dialysis have been increasing, ranging from 1% to 4%. Certain medications have also been implicated in the development of calciphylaxis, including warfarin, steroids, calcium-based phosphate binders, vitamin D, and iron. There is also an association with White individuals and more cases have been reported in females.
Pathophysiology of this condition includes calcification of the medial layer of arterioles and small arteries near the skin. Damage to vessel endothelium and formation of microthrombi contribute to the ischemia, which results in necrosis and ulceration of the skin. Elevated calcium and phosphate have been associated with these findings; however, these lab abnormalities alone are typically not enough to cause calciphylaxis. Vascular calcification inhibitors such as fetuin-A, osteoprotegerin, and matrix G1a protein may play a role in pathogenesis, with individuals lacking these factors potentially being at a greater risk. Specifically, matrix G1a protein is dependent on vitamin K dependent carboxylation, which may elucidate why warfarin has been implicated in the development of calciphylaxis because of interference with this pathway.
Upon presentation, patients will have painful ischemic plaques on the skin or painful subcutaneous nodules. Long-standing lesions may have a necrotic eschar or secondary infection, or may be associated with livedo reticularis. Areas with a greater concentration of adipose tissue such as the abdomen, thighs, and buttocks are most commonly affected, but lesions may appear anywhere. A biopsy may be done, but a clinical diagnosis is often sufficient as biopsies carry risks of prolonged healing and infection.
The differential diagnosis includes warfarin skin necrosis, cholesterol embolization, vasculitis, antiphospholipid syndrome, and cellulitis. Although this is a cutaneous manifestation, calciphylaxis is indicative of a systemic problem and requires multidisciplinary intervention.
Patients who present with calciphylaxis require a complete metabolic panel, liver function tests, coagulation studies, and albumin tests. Depending on the presentation, imaging studies such as nuclear medicine scans may be used if extensive soft tissue involvement is suspected.
Clinical management includes carefully avoiding electrolyte imbalances, initiating dialysis if necessary, discontinuing potentially offending supplements and medications, and administering proper wound care and pain management. Debridement of necrotic tissue may be necessary and should be initiated early as this has been associated with a 6-month increase in survival. Physicians should have a low threshold for starting antibiotics if secondary infection is suspected, but prophylaxis is not recommended. Sodium thiosulfate has been used off-label, but the mechanism of action is unknown and some meta-analyses indicate this treatment is not significantly associated with improvement of skin lesions. Interventions such as hyperbaric oxygen have also been used, but there is still more research to be done on these modalities.
The case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, Fort Lauderdale, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Kodumudi V et al. Adv Ther. 2020 Dec;37(12):4797-4807. doi: 10.1007/s12325-020-01504-w.
Seethapathy H et al. Adv Chronic Kidney Dis. 2019 Nov;26(6):484-490. doi: 10.1053/j.ackd.2019.09.005.
Turek M et al. Am J Case Rep. 2021 Jun 7:22:e930026. doi: 10.12659/AJCR.930026.
Wen W at al. JAMA Netw Open. 2023;6(4):e2310068. doi:10.1001/jamanetworkopen.2023.10068.
Westphal SG, Plumb T. Calciphylaxis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK519020/.
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare condition most commonly observed in patients with end-stage renal disease (ESRD). Because of the non-healing nature of the wounds and need for frequent hospitalizations, there is a significant risk of sepsis with a 1-year mortality rate greater than 50%.
Beyond ESRD, calciphylaxis is also associated with obesity, diabetes, hypoalbuminemia, autoimmune conditions, hepatic disease, malignancies, and dialysis. Rates in patients on dialysis have been increasing, ranging from 1% to 4%. Certain medications have also been implicated in the development of calciphylaxis, including warfarin, steroids, calcium-based phosphate binders, vitamin D, and iron. There is also an association with White individuals and more cases have been reported in females.
Pathophysiology of this condition includes calcification of the medial layer of arterioles and small arteries near the skin. Damage to vessel endothelium and formation of microthrombi contribute to the ischemia, which results in necrosis and ulceration of the skin. Elevated calcium and phosphate have been associated with these findings; however, these lab abnormalities alone are typically not enough to cause calciphylaxis. Vascular calcification inhibitors such as fetuin-A, osteoprotegerin, and matrix G1a protein may play a role in pathogenesis, with individuals lacking these factors potentially being at a greater risk. Specifically, matrix G1a protein is dependent on vitamin K dependent carboxylation, which may elucidate why warfarin has been implicated in the development of calciphylaxis because of interference with this pathway.
Upon presentation, patients will have painful ischemic plaques on the skin or painful subcutaneous nodules. Long-standing lesions may have a necrotic eschar or secondary infection, or may be associated with livedo reticularis. Areas with a greater concentration of adipose tissue such as the abdomen, thighs, and buttocks are most commonly affected, but lesions may appear anywhere. A biopsy may be done, but a clinical diagnosis is often sufficient as biopsies carry risks of prolonged healing and infection.
The differential diagnosis includes warfarin skin necrosis, cholesterol embolization, vasculitis, antiphospholipid syndrome, and cellulitis. Although this is a cutaneous manifestation, calciphylaxis is indicative of a systemic problem and requires multidisciplinary intervention.
Patients who present with calciphylaxis require a complete metabolic panel, liver function tests, coagulation studies, and albumin tests. Depending on the presentation, imaging studies such as nuclear medicine scans may be used if extensive soft tissue involvement is suspected.
Clinical management includes carefully avoiding electrolyte imbalances, initiating dialysis if necessary, discontinuing potentially offending supplements and medications, and administering proper wound care and pain management. Debridement of necrotic tissue may be necessary and should be initiated early as this has been associated with a 6-month increase in survival. Physicians should have a low threshold for starting antibiotics if secondary infection is suspected, but prophylaxis is not recommended. Sodium thiosulfate has been used off-label, but the mechanism of action is unknown and some meta-analyses indicate this treatment is not significantly associated with improvement of skin lesions. Interventions such as hyperbaric oxygen have also been used, but there is still more research to be done on these modalities.
The case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, Fort Lauderdale, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Kodumudi V et al. Adv Ther. 2020 Dec;37(12):4797-4807. doi: 10.1007/s12325-020-01504-w.
Seethapathy H et al. Adv Chronic Kidney Dis. 2019 Nov;26(6):484-490. doi: 10.1053/j.ackd.2019.09.005.
Turek M et al. Am J Case Rep. 2021 Jun 7:22:e930026. doi: 10.12659/AJCR.930026.
Wen W at al. JAMA Netw Open. 2023;6(4):e2310068. doi:10.1001/jamanetworkopen.2023.10068.
Westphal SG, Plumb T. Calciphylaxis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK519020/.
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare condition most commonly observed in patients with end-stage renal disease (ESRD). Because of the non-healing nature of the wounds and need for frequent hospitalizations, there is a significant risk of sepsis with a 1-year mortality rate greater than 50%.
Beyond ESRD, calciphylaxis is also associated with obesity, diabetes, hypoalbuminemia, autoimmune conditions, hepatic disease, malignancies, and dialysis. Rates in patients on dialysis have been increasing, ranging from 1% to 4%. Certain medications have also been implicated in the development of calciphylaxis, including warfarin, steroids, calcium-based phosphate binders, vitamin D, and iron. There is also an association with White individuals and more cases have been reported in females.
Pathophysiology of this condition includes calcification of the medial layer of arterioles and small arteries near the skin. Damage to vessel endothelium and formation of microthrombi contribute to the ischemia, which results in necrosis and ulceration of the skin. Elevated calcium and phosphate have been associated with these findings; however, these lab abnormalities alone are typically not enough to cause calciphylaxis. Vascular calcification inhibitors such as fetuin-A, osteoprotegerin, and matrix G1a protein may play a role in pathogenesis, with individuals lacking these factors potentially being at a greater risk. Specifically, matrix G1a protein is dependent on vitamin K dependent carboxylation, which may elucidate why warfarin has been implicated in the development of calciphylaxis because of interference with this pathway.
Upon presentation, patients will have painful ischemic plaques on the skin or painful subcutaneous nodules. Long-standing lesions may have a necrotic eschar or secondary infection, or may be associated with livedo reticularis. Areas with a greater concentration of adipose tissue such as the abdomen, thighs, and buttocks are most commonly affected, but lesions may appear anywhere. A biopsy may be done, but a clinical diagnosis is often sufficient as biopsies carry risks of prolonged healing and infection.
The differential diagnosis includes warfarin skin necrosis, cholesterol embolization, vasculitis, antiphospholipid syndrome, and cellulitis. Although this is a cutaneous manifestation, calciphylaxis is indicative of a systemic problem and requires multidisciplinary intervention.
Patients who present with calciphylaxis require a complete metabolic panel, liver function tests, coagulation studies, and albumin tests. Depending on the presentation, imaging studies such as nuclear medicine scans may be used if extensive soft tissue involvement is suspected.
Clinical management includes carefully avoiding electrolyte imbalances, initiating dialysis if necessary, discontinuing potentially offending supplements and medications, and administering proper wound care and pain management. Debridement of necrotic tissue may be necessary and should be initiated early as this has been associated with a 6-month increase in survival. Physicians should have a low threshold for starting antibiotics if secondary infection is suspected, but prophylaxis is not recommended. Sodium thiosulfate has been used off-label, but the mechanism of action is unknown and some meta-analyses indicate this treatment is not significantly associated with improvement of skin lesions. Interventions such as hyperbaric oxygen have also been used, but there is still more research to be done on these modalities.
The case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, Fort Lauderdale, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Kodumudi V et al. Adv Ther. 2020 Dec;37(12):4797-4807. doi: 10.1007/s12325-020-01504-w.
Seethapathy H et al. Adv Chronic Kidney Dis. 2019 Nov;26(6):484-490. doi: 10.1053/j.ackd.2019.09.005.
Turek M et al. Am J Case Rep. 2021 Jun 7:22:e930026. doi: 10.12659/AJCR.930026.
Wen W at al. JAMA Netw Open. 2023;6(4):e2310068. doi:10.1001/jamanetworkopen.2023.10068.
Westphal SG, Plumb T. Calciphylaxis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK519020/.
An 81-year-old White woman with a medical history significant for end stage renal disease (ESRD) on dialysis, diabetes, and a cerebrovascular accident presented with a 2-week history of a very painful lesion on her left calf. Upon physical exam, she was also noted to have tender subcutaneous nodules on her left anterolateral thigh that had been present for several weeks.
What's your diagnosis?
Special Considerations Needed in Applying Lupus Nephritis Guideline to Children
WASHINGTON — When the American College of Rheumatology (ACR) released its updated guideline for management of lupus nephritis (LN) at its 2024 Annual Meeting, they included recommendations for managing pediatric LN for the first time.
The pediatric recommendations use the same classification criteria, outcome measures, and treatments as in adults — including the first-line triple therapy recommendation — but there remain important differences between pediatric and adult LN, Mary Beth Son, MD, clinical chief of immunology and section chief of rheumatology at Boston Children’s Hospital in Massachusetts, and an associate professor of pediatrics at Harvard Medical School, also in Boston, told attendees.
“In general, kids and adolescents with lupus are sicker,” Son said. They are more likely to have renal manifestations and neuropsychiatric lupus at diagnosis, compared with adults. Further, “although the disease is the same, it’s happening to kids and adolescents who are undergoing critical periods of growth and development.”
Medication risk profiles also shift for younger patients, Son noted.
“Importantly, they’re at risk for higher cumulative dosing of both glucocorticoids and cyclophosphamide,” Son said. “When we give an adolescent a course of cyclophosphamide, we have to be aware that this might be the first of a few courses over the course of the lifetime disease, and with increasing numbers of cyclophosphamide courses, you have increased risk for infertility and malignancy.”
Son also acknowledged challenges of pediatric literature, including differences in definitions of pediatric lupus, very few randomized controlled trials, and fewer pediatric studies in general, with fewer participants. Given these research gaps, the guideline panels included pediatric rheumatologists and nephrologists, and the patient panel included several patients with childhood-onset disease.
Son also addressed differences in pediatric drug development. Dosing studies also do not always directly translate from adults to children because children have larger drug volume distribution and differences in drug clearance, and they may need different formulations, she said. Children tend to tolerate medications better than adults because they usually have fewer comorbidities, but the assessment of a drug’s safety must take its impact on growth and development into consideration.
During a press conference after the session where the guideline was presented, Linda Hiraki, MD, ScD, a clinician-scientist in rheumatology at the Hospital for Sick Children, Toronto, Ontario, Canada, said the panel took into consideration that pediatric patients receive their diagnosis during a critical time of development, so considerations of medication risks include the fact that children “have much more life to live.”
Triple Therapy Recommended
As with adults, the pediatric LN guideline recommends a triple therapy approach: glucocorticoids plus mycophenolate mofetil and belimumab, in addition to the usual renin-angiotensin-aldosterone system inhibitors and hydroxychloroquine. But Son acknowledged limitations of applying the new guideline to children. For one, voclosporin has not been studied in or approved for pediatric patients, although there exists modest evidence for other calcineurin inhibitors, mainly tacrolimus, in children.
“The other important consideration is that the lower dose of prednisone that’s being offered by the guidelines of 40 mg per day as a starting dose has not been studied in pediatric lupus nephritis patients,” Son said. “However, I would offer that, given that we know that kids get higher doses and longer courses, it’s even more important to consider a lower dose to begin with in the setting of other immunosuppressants.”
Good Practice Statements for Pediatric LN
Son also reviewed three good practice statements for pediatric LN. First, “glucocorticoid regimens should use pediatric-appropriate doses for children, as reduction of human glucocorticoid dosing is critically important given the early age of pediatric lupus onset and attendant comorbidities,” she said.
That statement is based on both common sense and some literature, including awareness that children are more likely to receive higher doses of steroids and that children’s higher damage scores are driven in part by steroid-related toxicity, such as avascular necrosis and cataracts. In addition, glucocorticoids can have profound effects on body mass index, mood, and height attainment.
“This is during a period of emerging self-identity and struggles with appearance; steroids exacerbate that” as well as mood issues already associated with puberty, Son said.
The second good practice statement recommends that clinicians monitor patients “for delayed pubertal onset and decreased growth velocity that can result from disease activity and glucocorticoid treatment and consider referral to pediatric endocrinology if indicated.” The third states that “a structured, intentional transition from pediatric to adult rheumatology care is indicated to avoid poor outcomes during this vulnerable period.”
During the press conference, Hiraki said that pediatric rheumatologists already recognize the need for discussions about transfer to adult care to begin very early, even years before patients are ready to transfer.
“The transition from being a pediatric patient to being an adult patient is very challenging for a number of reasons,” starting with loss of insurance coverage, added Bonnie Bermas, MD, a professor of internal medicine at UT Southwestern Medical Center in Dallas, Texas. When adult rheumatologists take on these patients, they may not have had care for 2 or 3 years, she said.
Rebecca Sadun, MD, PhD, an associate professor of pediatrics in rheumatology at Duke University School of Medicine, Durham, North Carolina, and vice-chair of the Systemic Lupus Erythematosus Committee for the Childhood Arthritis and Rheumatology Research Alliance, was not involved in the guideline development process but reviewed the new guideline.
“We appreciate that the ACR took care to involve pediatric rheumatologists, pediatric nephrologists, and patients with childhood-onset lupus in the development of the newest lupus nephritis treatment guidelines,” she said in an interview. She also noted, however, that “the dearth of pediatric-specific clinical trial data means that we continue to wonder when it is appropriate to extrapolate from adult data regarding the efficacy, safety, and dosing of certain medications, including steroids and voclosporin.” She also noted that voclosporin use can increase pill burden and therefore be difficult to use in pediatrics.
“Children, adolescents, and young adults are a unique population with unique challenges, including significant struggles with adherence to complex medication regimens,” she said. Sadun drew attention to two themes from the guideline that she found particularly applicable to management of pediatric LN.
“First, we must remain wary of the serious consequences of long-term, high-dose glucocorticoids, and we should continue to look towards steroid-sparing strategies that will reduce reliance on glucocorticoids,” Sadun said. “Second, we are likely to see better outcomes, including better renal response, when we take advantage of combination immunosuppression earlier in the disease course.”
Son, Bermas, and Sadun had no disclosures. Hiraki has consulted for Janssen. The guideline development did not involve outside funding.
A version of this article first appeared on Medscape.com.
WASHINGTON — When the American College of Rheumatology (ACR) released its updated guideline for management of lupus nephritis (LN) at its 2024 Annual Meeting, they included recommendations for managing pediatric LN for the first time.
The pediatric recommendations use the same classification criteria, outcome measures, and treatments as in adults — including the first-line triple therapy recommendation — but there remain important differences between pediatric and adult LN, Mary Beth Son, MD, clinical chief of immunology and section chief of rheumatology at Boston Children’s Hospital in Massachusetts, and an associate professor of pediatrics at Harvard Medical School, also in Boston, told attendees.
“In general, kids and adolescents with lupus are sicker,” Son said. They are more likely to have renal manifestations and neuropsychiatric lupus at diagnosis, compared with adults. Further, “although the disease is the same, it’s happening to kids and adolescents who are undergoing critical periods of growth and development.”
Medication risk profiles also shift for younger patients, Son noted.
“Importantly, they’re at risk for higher cumulative dosing of both glucocorticoids and cyclophosphamide,” Son said. “When we give an adolescent a course of cyclophosphamide, we have to be aware that this might be the first of a few courses over the course of the lifetime disease, and with increasing numbers of cyclophosphamide courses, you have increased risk for infertility and malignancy.”
Son also acknowledged challenges of pediatric literature, including differences in definitions of pediatric lupus, very few randomized controlled trials, and fewer pediatric studies in general, with fewer participants. Given these research gaps, the guideline panels included pediatric rheumatologists and nephrologists, and the patient panel included several patients with childhood-onset disease.
Son also addressed differences in pediatric drug development. Dosing studies also do not always directly translate from adults to children because children have larger drug volume distribution and differences in drug clearance, and they may need different formulations, she said. Children tend to tolerate medications better than adults because they usually have fewer comorbidities, but the assessment of a drug’s safety must take its impact on growth and development into consideration.
During a press conference after the session where the guideline was presented, Linda Hiraki, MD, ScD, a clinician-scientist in rheumatology at the Hospital for Sick Children, Toronto, Ontario, Canada, said the panel took into consideration that pediatric patients receive their diagnosis during a critical time of development, so considerations of medication risks include the fact that children “have much more life to live.”
Triple Therapy Recommended
As with adults, the pediatric LN guideline recommends a triple therapy approach: glucocorticoids plus mycophenolate mofetil and belimumab, in addition to the usual renin-angiotensin-aldosterone system inhibitors and hydroxychloroquine. But Son acknowledged limitations of applying the new guideline to children. For one, voclosporin has not been studied in or approved for pediatric patients, although there exists modest evidence for other calcineurin inhibitors, mainly tacrolimus, in children.
“The other important consideration is that the lower dose of prednisone that’s being offered by the guidelines of 40 mg per day as a starting dose has not been studied in pediatric lupus nephritis patients,” Son said. “However, I would offer that, given that we know that kids get higher doses and longer courses, it’s even more important to consider a lower dose to begin with in the setting of other immunosuppressants.”
Good Practice Statements for Pediatric LN
Son also reviewed three good practice statements for pediatric LN. First, “glucocorticoid regimens should use pediatric-appropriate doses for children, as reduction of human glucocorticoid dosing is critically important given the early age of pediatric lupus onset and attendant comorbidities,” she said.
That statement is based on both common sense and some literature, including awareness that children are more likely to receive higher doses of steroids and that children’s higher damage scores are driven in part by steroid-related toxicity, such as avascular necrosis and cataracts. In addition, glucocorticoids can have profound effects on body mass index, mood, and height attainment.
“This is during a period of emerging self-identity and struggles with appearance; steroids exacerbate that” as well as mood issues already associated with puberty, Son said.
The second good practice statement recommends that clinicians monitor patients “for delayed pubertal onset and decreased growth velocity that can result from disease activity and glucocorticoid treatment and consider referral to pediatric endocrinology if indicated.” The third states that “a structured, intentional transition from pediatric to adult rheumatology care is indicated to avoid poor outcomes during this vulnerable period.”
During the press conference, Hiraki said that pediatric rheumatologists already recognize the need for discussions about transfer to adult care to begin very early, even years before patients are ready to transfer.
“The transition from being a pediatric patient to being an adult patient is very challenging for a number of reasons,” starting with loss of insurance coverage, added Bonnie Bermas, MD, a professor of internal medicine at UT Southwestern Medical Center in Dallas, Texas. When adult rheumatologists take on these patients, they may not have had care for 2 or 3 years, she said.
Rebecca Sadun, MD, PhD, an associate professor of pediatrics in rheumatology at Duke University School of Medicine, Durham, North Carolina, and vice-chair of the Systemic Lupus Erythematosus Committee for the Childhood Arthritis and Rheumatology Research Alliance, was not involved in the guideline development process but reviewed the new guideline.
“We appreciate that the ACR took care to involve pediatric rheumatologists, pediatric nephrologists, and patients with childhood-onset lupus in the development of the newest lupus nephritis treatment guidelines,” she said in an interview. She also noted, however, that “the dearth of pediatric-specific clinical trial data means that we continue to wonder when it is appropriate to extrapolate from adult data regarding the efficacy, safety, and dosing of certain medications, including steroids and voclosporin.” She also noted that voclosporin use can increase pill burden and therefore be difficult to use in pediatrics.
“Children, adolescents, and young adults are a unique population with unique challenges, including significant struggles with adherence to complex medication regimens,” she said. Sadun drew attention to two themes from the guideline that she found particularly applicable to management of pediatric LN.
“First, we must remain wary of the serious consequences of long-term, high-dose glucocorticoids, and we should continue to look towards steroid-sparing strategies that will reduce reliance on glucocorticoids,” Sadun said. “Second, we are likely to see better outcomes, including better renal response, when we take advantage of combination immunosuppression earlier in the disease course.”
Son, Bermas, and Sadun had no disclosures. Hiraki has consulted for Janssen. The guideline development did not involve outside funding.
A version of this article first appeared on Medscape.com.
WASHINGTON — When the American College of Rheumatology (ACR) released its updated guideline for management of lupus nephritis (LN) at its 2024 Annual Meeting, they included recommendations for managing pediatric LN for the first time.
The pediatric recommendations use the same classification criteria, outcome measures, and treatments as in adults — including the first-line triple therapy recommendation — but there remain important differences between pediatric and adult LN, Mary Beth Son, MD, clinical chief of immunology and section chief of rheumatology at Boston Children’s Hospital in Massachusetts, and an associate professor of pediatrics at Harvard Medical School, also in Boston, told attendees.
“In general, kids and adolescents with lupus are sicker,” Son said. They are more likely to have renal manifestations and neuropsychiatric lupus at diagnosis, compared with adults. Further, “although the disease is the same, it’s happening to kids and adolescents who are undergoing critical periods of growth and development.”
Medication risk profiles also shift for younger patients, Son noted.
“Importantly, they’re at risk for higher cumulative dosing of both glucocorticoids and cyclophosphamide,” Son said. “When we give an adolescent a course of cyclophosphamide, we have to be aware that this might be the first of a few courses over the course of the lifetime disease, and with increasing numbers of cyclophosphamide courses, you have increased risk for infertility and malignancy.”
Son also acknowledged challenges of pediatric literature, including differences in definitions of pediatric lupus, very few randomized controlled trials, and fewer pediatric studies in general, with fewer participants. Given these research gaps, the guideline panels included pediatric rheumatologists and nephrologists, and the patient panel included several patients with childhood-onset disease.
Son also addressed differences in pediatric drug development. Dosing studies also do not always directly translate from adults to children because children have larger drug volume distribution and differences in drug clearance, and they may need different formulations, she said. Children tend to tolerate medications better than adults because they usually have fewer comorbidities, but the assessment of a drug’s safety must take its impact on growth and development into consideration.
During a press conference after the session where the guideline was presented, Linda Hiraki, MD, ScD, a clinician-scientist in rheumatology at the Hospital for Sick Children, Toronto, Ontario, Canada, said the panel took into consideration that pediatric patients receive their diagnosis during a critical time of development, so considerations of medication risks include the fact that children “have much more life to live.”
Triple Therapy Recommended
As with adults, the pediatric LN guideline recommends a triple therapy approach: glucocorticoids plus mycophenolate mofetil and belimumab, in addition to the usual renin-angiotensin-aldosterone system inhibitors and hydroxychloroquine. But Son acknowledged limitations of applying the new guideline to children. For one, voclosporin has not been studied in or approved for pediatric patients, although there exists modest evidence for other calcineurin inhibitors, mainly tacrolimus, in children.
“The other important consideration is that the lower dose of prednisone that’s being offered by the guidelines of 40 mg per day as a starting dose has not been studied in pediatric lupus nephritis patients,” Son said. “However, I would offer that, given that we know that kids get higher doses and longer courses, it’s even more important to consider a lower dose to begin with in the setting of other immunosuppressants.”
Good Practice Statements for Pediatric LN
Son also reviewed three good practice statements for pediatric LN. First, “glucocorticoid regimens should use pediatric-appropriate doses for children, as reduction of human glucocorticoid dosing is critically important given the early age of pediatric lupus onset and attendant comorbidities,” she said.
That statement is based on both common sense and some literature, including awareness that children are more likely to receive higher doses of steroids and that children’s higher damage scores are driven in part by steroid-related toxicity, such as avascular necrosis and cataracts. In addition, glucocorticoids can have profound effects on body mass index, mood, and height attainment.
“This is during a period of emerging self-identity and struggles with appearance; steroids exacerbate that” as well as mood issues already associated with puberty, Son said.
The second good practice statement recommends that clinicians monitor patients “for delayed pubertal onset and decreased growth velocity that can result from disease activity and glucocorticoid treatment and consider referral to pediatric endocrinology if indicated.” The third states that “a structured, intentional transition from pediatric to adult rheumatology care is indicated to avoid poor outcomes during this vulnerable period.”
During the press conference, Hiraki said that pediatric rheumatologists already recognize the need for discussions about transfer to adult care to begin very early, even years before patients are ready to transfer.
“The transition from being a pediatric patient to being an adult patient is very challenging for a number of reasons,” starting with loss of insurance coverage, added Bonnie Bermas, MD, a professor of internal medicine at UT Southwestern Medical Center in Dallas, Texas. When adult rheumatologists take on these patients, they may not have had care for 2 or 3 years, she said.
Rebecca Sadun, MD, PhD, an associate professor of pediatrics in rheumatology at Duke University School of Medicine, Durham, North Carolina, and vice-chair of the Systemic Lupus Erythematosus Committee for the Childhood Arthritis and Rheumatology Research Alliance, was not involved in the guideline development process but reviewed the new guideline.
“We appreciate that the ACR took care to involve pediatric rheumatologists, pediatric nephrologists, and patients with childhood-onset lupus in the development of the newest lupus nephritis treatment guidelines,” she said in an interview. She also noted, however, that “the dearth of pediatric-specific clinical trial data means that we continue to wonder when it is appropriate to extrapolate from adult data regarding the efficacy, safety, and dosing of certain medications, including steroids and voclosporin.” She also noted that voclosporin use can increase pill burden and therefore be difficult to use in pediatrics.
“Children, adolescents, and young adults are a unique population with unique challenges, including significant struggles with adherence to complex medication regimens,” she said. Sadun drew attention to two themes from the guideline that she found particularly applicable to management of pediatric LN.
“First, we must remain wary of the serious consequences of long-term, high-dose glucocorticoids, and we should continue to look towards steroid-sparing strategies that will reduce reliance on glucocorticoids,” Sadun said. “Second, we are likely to see better outcomes, including better renal response, when we take advantage of combination immunosuppression earlier in the disease course.”
Son, Bermas, and Sadun had no disclosures. Hiraki has consulted for Janssen. The guideline development did not involve outside funding.
A version of this article first appeared on Medscape.com.
FROM ACR 2024
Could a Urinary Biomarker Panel Be a ‘Game Changer’ for Lupus Nephritis Management?
WASHINGTON — An investigational 12-protein panel of urinary biomarkers predicted histologically active lupus nephritis (LN) with 86% accuracy, according to research presented at the American College of Rheumatology (ACR) 2024 Annual Meeting.
The noninvasive biomarker panel “robustly predicts meaningful and actionable histological findings” in patients with active proliferative LN, Andrea Fava, MD, assistant professor of medicine in the Division of Rheumatology at Johns Hopkins Medicine in Baltimore, told attendees.
“In contrast to proteinuria, which can’t differentiate inflammation from damage, this panel for histological activity includes a set of 12 proteins linked to intrarenal inflammation,” said Fava, director of Lupus Translational Research at Johns Hopkins. A decline in the biomarker score at 3 months predicted a clinical response at 1 year, and persistent elevation of the score at 1 year predicted permanent loss of kidney function, “which makes it tempting as a treatment endpoint,” Fava said. “Upon further validation, this biomarker panel could aid in the diagnosis of lupus nephritis and guide treatment decisions.”
Alfred Kim, MD, PhD, an associate professor of medicine at Washington University in St. Louis, was not involved in the research but noted the potential value of a reliable biomarker panel.
“If we have urinary biomarkers that strongly associate with histologic activity, this would be a game changer in the management of LN,” Kim told Medscape Medical News. “Right now, the gold standard is to perform another kidney biopsy to determine if therapy is working. But this is invasive, and many patients do not want to do another kidney biopsy. Conversely, the easiest way to assess lupus nephritis activity is through a urinalysis, focusing on urinary protein levels,” but relying on proteinuria has limitations as well.
“The most important [limitation] is that proteinuria cannot distinguish treatable inflammation from chronic damage,” Fava said. Persistent histologic activity in patients without proteinuria predicts flares, but tracking histologic activity, as Kim noted, requires repeat biopsies.
“So we need better biomarkers because biomarkers that can reflect tissue biology in real time can guide personalized treatment, and that’s one of the main goals of the Accelerating Medicines Partnership [AMP],” he said. The AMP is a public-private partnership between the National Institutes of Health (NIH), the US Food and Drug Administration (FDA), multiple biopharmaceutical and life science companies, and nonprofit and other organizations. Lupus is one of the AMP’s funded projects.
Kim agreed that “effective biomarkers are a huge unmet need in LN.” Further, he said, “imagine a world where the diagnosis of LN can be made just through urinary biomarkers and obviate the need for biopsy. Both patients and providers will be ecstatic at this possibility.”
Fava described the background for how his research team determined what biomarkers to test. They had previously enrolled 225 patients with LN undergoing a clinically indicated kidney biopsy and collected urine samples from them at baseline and at 12, 24, and 52 weeks after their biopsy.
Of the 225 patients included, 9% with only mesangial LN (class I-II), 25% with pure membranous LN (class V), 24% with mixed LN (class III or IV with or without V), 38% with proliferative LN (class III or IV), and 4% with advanced sclerosis LN (class VI). From these samples, they quantified 1200 proteins and looked at how they correlated with histologic activity.
“What was interesting was that in patients who were classified as responders after 1 year, there were many of these proteins that declined as early as 3 months, suggesting that effective immunosuppression is reducing intrarenal inflammation, and we can capture it in real time,” Fava said.
Biomarker Panel Predicts Histologically Active LN
So they set to determining whether they could develop a urinary biomarker for histologically active LN that could be useful in clinical decision-making. They focused on one that could detect active proliferative LN with an NIH activity index score > 2. Their 179 participants included 47.5% Black, 27.9% White, and 14.5% Asian participants, with 10.1% of other races. The predominantly female (86.6%) cohort had an average age of 37 years. Among the LN classes, about one third (34.6%) had pure proliferative disease, 17.9% had mixed proliferative, 27.9% had pure membranous, 11.7% had class I or II, and 5% had class VI. Just over half the participants (55.7%) had not responded to treatment at 12 months, whereas 25% had a complete response, and 19.3% had a partial response.
However, both the 78 participants with an NIH activity index score > 2 and the 101 with a score ≤ 2 had a median score of 3 on the NIH chronicity index. And the urine protein-to-creatinine ratio — 2.8 in the group with an NIH activity index score > 2 and 2.4 in the other group — was nearly indistinguishable between the two groups, Fava said.
They then trained multiple algorithms on 80% of the data to find the best performing set of proteins (with an area under the curve [AUC] of 90%) for predicting an NIH activity index score > 2. They reduced the number of proteins to maximize practicality and performance of the panel, Fava said, and ultimately identified a 12-protein panel that was highly predictive of an NIH activity index score > 2. Then, they validated that panel using the other 20% of the data. The training set had an AUC of 90%, and the test set was validated with an AUC of 93%.
The 12-protein panel score outperformed anti-dsDNA, C3 complement, and proteinuria, with a sensitivity of 81%, a specificity of 90%, a positive predictive value of 87%, a negative predictive value of 86%, and an accuracy of 86%. The proteins with the greatest relative importance were CD163, cathepsin S, FOLR2, and CEACAM-1.
“In contrast to proteinuria, these proteins were related to inflammatory processes found in the kidneys in patients with lupus nephritis, such as activation of macrophages, neutrophils and monocytes, lymphocytes, and complement,” Fava said.
When they looked at the trajectories of the probabilities from the biomarker panel at 3, 6, and 12 months, the probability of the NIH activity index score remaining > 2 stayed high in the nonresponders over 1 year, but the trajectory declined at 3 months in the responders, indicating a decrease in kidney inflammation (P < .001).
Can the Biomarker Panel Serve as a Treatment Endpoint?
Then, to determine whether the panel could act as a reliable treatment endpoint, the researchers followed the patients for up to 7 years. One third of the patients lost more than 40% of their kidney function during the follow-up. They found that a high urinary biomarker score at 12 months predicted future glomerular filtration rate loss, independent of proteinuria.
This panel was tested specifically for proliferative LN, so “we may need distinct panels for each [LN type] to capture most of these patients,” Kim said. “I think that’s where the gold mine is: A personalized medicine approach where a large biomarker panel identifies which smaller panel that patient best fits, then use that for monitoring.”
Kim did note an important potential limitation in the study regarding how samples are used in biomarker discovery and validation vs in clinical practice. “Most samples in research studies are frozen, then thawed, while urine is assayed within a couple hours after collection in the clinical setting,” he said. “Do sample processing differences create a situation where a biomarker works in a research project but not in the clinical setting?” But more likely, he said, the opposite may be the case, where frozen samples allow for more degradation of proteins and potentially useful LN biomarker candidates are never detected.
Another challenge, Kim added, albeit unrelated to the study findings, is that diagnostic companies are finding it difficult to get payers to cover new tests, so that could become a challenge if the panel undergoes further validation and then FDA qualification.
The research was funded by Exagen. Fava reported disclosures with Arctiva, AstraZeneca, Exagen, Novartis, UCB, Bristol Myers Squibb, Annexon Bio, and Bain Capital. His coauthors reported financial relationships with numerous pharmaceutical and life science companies, including Exagen, and some are employees of Exagen.
Kim reported research agreements with AstraZeneca, Bristol Myers Squibb, Novartis, and CRISPR Therapeutics; receiving royalties from Kypha; and receiving consulting/speaking fees from AbbVie, Amgen, Atara Bio, Aurinia, Cargo Tx, Exagen, GlaxoSmithKline, Hinge Bio, Kypha, and UpToDate.
A version of this article appeared on Medscape.com.
WASHINGTON — An investigational 12-protein panel of urinary biomarkers predicted histologically active lupus nephritis (LN) with 86% accuracy, according to research presented at the American College of Rheumatology (ACR) 2024 Annual Meeting.
The noninvasive biomarker panel “robustly predicts meaningful and actionable histological findings” in patients with active proliferative LN, Andrea Fava, MD, assistant professor of medicine in the Division of Rheumatology at Johns Hopkins Medicine in Baltimore, told attendees.
“In contrast to proteinuria, which can’t differentiate inflammation from damage, this panel for histological activity includes a set of 12 proteins linked to intrarenal inflammation,” said Fava, director of Lupus Translational Research at Johns Hopkins. A decline in the biomarker score at 3 months predicted a clinical response at 1 year, and persistent elevation of the score at 1 year predicted permanent loss of kidney function, “which makes it tempting as a treatment endpoint,” Fava said. “Upon further validation, this biomarker panel could aid in the diagnosis of lupus nephritis and guide treatment decisions.”
Alfred Kim, MD, PhD, an associate professor of medicine at Washington University in St. Louis, was not involved in the research but noted the potential value of a reliable biomarker panel.
“If we have urinary biomarkers that strongly associate with histologic activity, this would be a game changer in the management of LN,” Kim told Medscape Medical News. “Right now, the gold standard is to perform another kidney biopsy to determine if therapy is working. But this is invasive, and many patients do not want to do another kidney biopsy. Conversely, the easiest way to assess lupus nephritis activity is through a urinalysis, focusing on urinary protein levels,” but relying on proteinuria has limitations as well.
“The most important [limitation] is that proteinuria cannot distinguish treatable inflammation from chronic damage,” Fava said. Persistent histologic activity in patients without proteinuria predicts flares, but tracking histologic activity, as Kim noted, requires repeat biopsies.
“So we need better biomarkers because biomarkers that can reflect tissue biology in real time can guide personalized treatment, and that’s one of the main goals of the Accelerating Medicines Partnership [AMP],” he said. The AMP is a public-private partnership between the National Institutes of Health (NIH), the US Food and Drug Administration (FDA), multiple biopharmaceutical and life science companies, and nonprofit and other organizations. Lupus is one of the AMP’s funded projects.
Kim agreed that “effective biomarkers are a huge unmet need in LN.” Further, he said, “imagine a world where the diagnosis of LN can be made just through urinary biomarkers and obviate the need for biopsy. Both patients and providers will be ecstatic at this possibility.”
Fava described the background for how his research team determined what biomarkers to test. They had previously enrolled 225 patients with LN undergoing a clinically indicated kidney biopsy and collected urine samples from them at baseline and at 12, 24, and 52 weeks after their biopsy.
Of the 225 patients included, 9% with only mesangial LN (class I-II), 25% with pure membranous LN (class V), 24% with mixed LN (class III or IV with or without V), 38% with proliferative LN (class III or IV), and 4% with advanced sclerosis LN (class VI). From these samples, they quantified 1200 proteins and looked at how they correlated with histologic activity.
“What was interesting was that in patients who were classified as responders after 1 year, there were many of these proteins that declined as early as 3 months, suggesting that effective immunosuppression is reducing intrarenal inflammation, and we can capture it in real time,” Fava said.
Biomarker Panel Predicts Histologically Active LN
So they set to determining whether they could develop a urinary biomarker for histologically active LN that could be useful in clinical decision-making. They focused on one that could detect active proliferative LN with an NIH activity index score > 2. Their 179 participants included 47.5% Black, 27.9% White, and 14.5% Asian participants, with 10.1% of other races. The predominantly female (86.6%) cohort had an average age of 37 years. Among the LN classes, about one third (34.6%) had pure proliferative disease, 17.9% had mixed proliferative, 27.9% had pure membranous, 11.7% had class I or II, and 5% had class VI. Just over half the participants (55.7%) had not responded to treatment at 12 months, whereas 25% had a complete response, and 19.3% had a partial response.
However, both the 78 participants with an NIH activity index score > 2 and the 101 with a score ≤ 2 had a median score of 3 on the NIH chronicity index. And the urine protein-to-creatinine ratio — 2.8 in the group with an NIH activity index score > 2 and 2.4 in the other group — was nearly indistinguishable between the two groups, Fava said.
They then trained multiple algorithms on 80% of the data to find the best performing set of proteins (with an area under the curve [AUC] of 90%) for predicting an NIH activity index score > 2. They reduced the number of proteins to maximize practicality and performance of the panel, Fava said, and ultimately identified a 12-protein panel that was highly predictive of an NIH activity index score > 2. Then, they validated that panel using the other 20% of the data. The training set had an AUC of 90%, and the test set was validated with an AUC of 93%.
The 12-protein panel score outperformed anti-dsDNA, C3 complement, and proteinuria, with a sensitivity of 81%, a specificity of 90%, a positive predictive value of 87%, a negative predictive value of 86%, and an accuracy of 86%. The proteins with the greatest relative importance were CD163, cathepsin S, FOLR2, and CEACAM-1.
“In contrast to proteinuria, these proteins were related to inflammatory processes found in the kidneys in patients with lupus nephritis, such as activation of macrophages, neutrophils and monocytes, lymphocytes, and complement,” Fava said.
When they looked at the trajectories of the probabilities from the biomarker panel at 3, 6, and 12 months, the probability of the NIH activity index score remaining > 2 stayed high in the nonresponders over 1 year, but the trajectory declined at 3 months in the responders, indicating a decrease in kidney inflammation (P < .001).
Can the Biomarker Panel Serve as a Treatment Endpoint?
Then, to determine whether the panel could act as a reliable treatment endpoint, the researchers followed the patients for up to 7 years. One third of the patients lost more than 40% of their kidney function during the follow-up. They found that a high urinary biomarker score at 12 months predicted future glomerular filtration rate loss, independent of proteinuria.
This panel was tested specifically for proliferative LN, so “we may need distinct panels for each [LN type] to capture most of these patients,” Kim said. “I think that’s where the gold mine is: A personalized medicine approach where a large biomarker panel identifies which smaller panel that patient best fits, then use that for monitoring.”
Kim did note an important potential limitation in the study regarding how samples are used in biomarker discovery and validation vs in clinical practice. “Most samples in research studies are frozen, then thawed, while urine is assayed within a couple hours after collection in the clinical setting,” he said. “Do sample processing differences create a situation where a biomarker works in a research project but not in the clinical setting?” But more likely, he said, the opposite may be the case, where frozen samples allow for more degradation of proteins and potentially useful LN biomarker candidates are never detected.
Another challenge, Kim added, albeit unrelated to the study findings, is that diagnostic companies are finding it difficult to get payers to cover new tests, so that could become a challenge if the panel undergoes further validation and then FDA qualification.
The research was funded by Exagen. Fava reported disclosures with Arctiva, AstraZeneca, Exagen, Novartis, UCB, Bristol Myers Squibb, Annexon Bio, and Bain Capital. His coauthors reported financial relationships with numerous pharmaceutical and life science companies, including Exagen, and some are employees of Exagen.
Kim reported research agreements with AstraZeneca, Bristol Myers Squibb, Novartis, and CRISPR Therapeutics; receiving royalties from Kypha; and receiving consulting/speaking fees from AbbVie, Amgen, Atara Bio, Aurinia, Cargo Tx, Exagen, GlaxoSmithKline, Hinge Bio, Kypha, and UpToDate.
A version of this article appeared on Medscape.com.
WASHINGTON — An investigational 12-protein panel of urinary biomarkers predicted histologically active lupus nephritis (LN) with 86% accuracy, according to research presented at the American College of Rheumatology (ACR) 2024 Annual Meeting.
The noninvasive biomarker panel “robustly predicts meaningful and actionable histological findings” in patients with active proliferative LN, Andrea Fava, MD, assistant professor of medicine in the Division of Rheumatology at Johns Hopkins Medicine in Baltimore, told attendees.
“In contrast to proteinuria, which can’t differentiate inflammation from damage, this panel for histological activity includes a set of 12 proteins linked to intrarenal inflammation,” said Fava, director of Lupus Translational Research at Johns Hopkins. A decline in the biomarker score at 3 months predicted a clinical response at 1 year, and persistent elevation of the score at 1 year predicted permanent loss of kidney function, “which makes it tempting as a treatment endpoint,” Fava said. “Upon further validation, this biomarker panel could aid in the diagnosis of lupus nephritis and guide treatment decisions.”
Alfred Kim, MD, PhD, an associate professor of medicine at Washington University in St. Louis, was not involved in the research but noted the potential value of a reliable biomarker panel.
“If we have urinary biomarkers that strongly associate with histologic activity, this would be a game changer in the management of LN,” Kim told Medscape Medical News. “Right now, the gold standard is to perform another kidney biopsy to determine if therapy is working. But this is invasive, and many patients do not want to do another kidney biopsy. Conversely, the easiest way to assess lupus nephritis activity is through a urinalysis, focusing on urinary protein levels,” but relying on proteinuria has limitations as well.
“The most important [limitation] is that proteinuria cannot distinguish treatable inflammation from chronic damage,” Fava said. Persistent histologic activity in patients without proteinuria predicts flares, but tracking histologic activity, as Kim noted, requires repeat biopsies.
“So we need better biomarkers because biomarkers that can reflect tissue biology in real time can guide personalized treatment, and that’s one of the main goals of the Accelerating Medicines Partnership [AMP],” he said. The AMP is a public-private partnership between the National Institutes of Health (NIH), the US Food and Drug Administration (FDA), multiple biopharmaceutical and life science companies, and nonprofit and other organizations. Lupus is one of the AMP’s funded projects.
Kim agreed that “effective biomarkers are a huge unmet need in LN.” Further, he said, “imagine a world where the diagnosis of LN can be made just through urinary biomarkers and obviate the need for biopsy. Both patients and providers will be ecstatic at this possibility.”
Fava described the background for how his research team determined what biomarkers to test. They had previously enrolled 225 patients with LN undergoing a clinically indicated kidney biopsy and collected urine samples from them at baseline and at 12, 24, and 52 weeks after their biopsy.
Of the 225 patients included, 9% with only mesangial LN (class I-II), 25% with pure membranous LN (class V), 24% with mixed LN (class III or IV with or without V), 38% with proliferative LN (class III or IV), and 4% with advanced sclerosis LN (class VI). From these samples, they quantified 1200 proteins and looked at how they correlated with histologic activity.
“What was interesting was that in patients who were classified as responders after 1 year, there were many of these proteins that declined as early as 3 months, suggesting that effective immunosuppression is reducing intrarenal inflammation, and we can capture it in real time,” Fava said.
Biomarker Panel Predicts Histologically Active LN
So they set to determining whether they could develop a urinary biomarker for histologically active LN that could be useful in clinical decision-making. They focused on one that could detect active proliferative LN with an NIH activity index score > 2. Their 179 participants included 47.5% Black, 27.9% White, and 14.5% Asian participants, with 10.1% of other races. The predominantly female (86.6%) cohort had an average age of 37 years. Among the LN classes, about one third (34.6%) had pure proliferative disease, 17.9% had mixed proliferative, 27.9% had pure membranous, 11.7% had class I or II, and 5% had class VI. Just over half the participants (55.7%) had not responded to treatment at 12 months, whereas 25% had a complete response, and 19.3% had a partial response.
However, both the 78 participants with an NIH activity index score > 2 and the 101 with a score ≤ 2 had a median score of 3 on the NIH chronicity index. And the urine protein-to-creatinine ratio — 2.8 in the group with an NIH activity index score > 2 and 2.4 in the other group — was nearly indistinguishable between the two groups, Fava said.
They then trained multiple algorithms on 80% of the data to find the best performing set of proteins (with an area under the curve [AUC] of 90%) for predicting an NIH activity index score > 2. They reduced the number of proteins to maximize practicality and performance of the panel, Fava said, and ultimately identified a 12-protein panel that was highly predictive of an NIH activity index score > 2. Then, they validated that panel using the other 20% of the data. The training set had an AUC of 90%, and the test set was validated with an AUC of 93%.
The 12-protein panel score outperformed anti-dsDNA, C3 complement, and proteinuria, with a sensitivity of 81%, a specificity of 90%, a positive predictive value of 87%, a negative predictive value of 86%, and an accuracy of 86%. The proteins with the greatest relative importance were CD163, cathepsin S, FOLR2, and CEACAM-1.
“In contrast to proteinuria, these proteins were related to inflammatory processes found in the kidneys in patients with lupus nephritis, such as activation of macrophages, neutrophils and monocytes, lymphocytes, and complement,” Fava said.
When they looked at the trajectories of the probabilities from the biomarker panel at 3, 6, and 12 months, the probability of the NIH activity index score remaining > 2 stayed high in the nonresponders over 1 year, but the trajectory declined at 3 months in the responders, indicating a decrease in kidney inflammation (P < .001).
Can the Biomarker Panel Serve as a Treatment Endpoint?
Then, to determine whether the panel could act as a reliable treatment endpoint, the researchers followed the patients for up to 7 years. One third of the patients lost more than 40% of their kidney function during the follow-up. They found that a high urinary biomarker score at 12 months predicted future glomerular filtration rate loss, independent of proteinuria.
This panel was tested specifically for proliferative LN, so “we may need distinct panels for each [LN type] to capture most of these patients,” Kim said. “I think that’s where the gold mine is: A personalized medicine approach where a large biomarker panel identifies which smaller panel that patient best fits, then use that for monitoring.”
Kim did note an important potential limitation in the study regarding how samples are used in biomarker discovery and validation vs in clinical practice. “Most samples in research studies are frozen, then thawed, while urine is assayed within a couple hours after collection in the clinical setting,” he said. “Do sample processing differences create a situation where a biomarker works in a research project but not in the clinical setting?” But more likely, he said, the opposite may be the case, where frozen samples allow for more degradation of proteins and potentially useful LN biomarker candidates are never detected.
Another challenge, Kim added, albeit unrelated to the study findings, is that diagnostic companies are finding it difficult to get payers to cover new tests, so that could become a challenge if the panel undergoes further validation and then FDA qualification.
The research was funded by Exagen. Fava reported disclosures with Arctiva, AstraZeneca, Exagen, Novartis, UCB, Bristol Myers Squibb, Annexon Bio, and Bain Capital. His coauthors reported financial relationships with numerous pharmaceutical and life science companies, including Exagen, and some are employees of Exagen.
Kim reported research agreements with AstraZeneca, Bristol Myers Squibb, Novartis, and CRISPR Therapeutics; receiving royalties from Kypha; and receiving consulting/speaking fees from AbbVie, Amgen, Atara Bio, Aurinia, Cargo Tx, Exagen, GlaxoSmithKline, Hinge Bio, Kypha, and UpToDate.
A version of this article appeared on Medscape.com.
FROM ACR 2024






