User login
Agitation and emotional lability
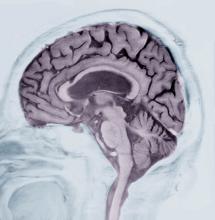
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 76-year-old Black woman presents to her physician. She is accompanied by her daughter who reports that, over the last 9 months, her mother has exhibited worsening memory loss, confusion, impaired judgment, agitation, and emotional lability. She is often unaware of where she is or how she got there. She sometimes does not recognize her family members or people who are familiar to her. Her appetite has been variable, and her sleep schedule is altered so that she often sleeps during the day and is awake at night. Sometimes, she is so irritable that she becomes aggressive and insists on situations that don’t exist. Her executive function is low. Her daughter reports that the patient had a fall 9 months ago and again 4 months ago, after which her symptoms became progressively worse.
The patient has complained about being forgetful and clumsy for much of the past 5 years, which she has attributed to old age. Until the last year or so, these have not greatly impaired her daily function and were not of great concern to her family or providers. She has a history of hypertension and diabetes, both of which are pharmacologically managed with mixed results due to variable adherence.
Physical exam confirms her daughter’s report. The patient appears thin, fatigued, and anxious. She has lost 20 lb since her last visit. She has great difficulty maintaining focus on what is being asked of her and in following the conversation. When she does speak, her speech is slow. She exhibits both motor deficits — in balance and coordination — and a bradykinetic gait.
Laboratory testing is performed: complete blood count w/diff, comprehensive metabolic panel, thyroid panel, cobalamin level, vitamin D screening. All results are within normal range for this patient. She was unable to complete the Geriatric Depression Scale on her own; direct questioning about whether she was feeling depressed is negative. Mini-Mental State Examination (MMSE) score is 18. MRI is performed; sagittal view reveals cortical atrophy.
Alzheimer's Disease Signs and Symptoms
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Fatigue and brain fog
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
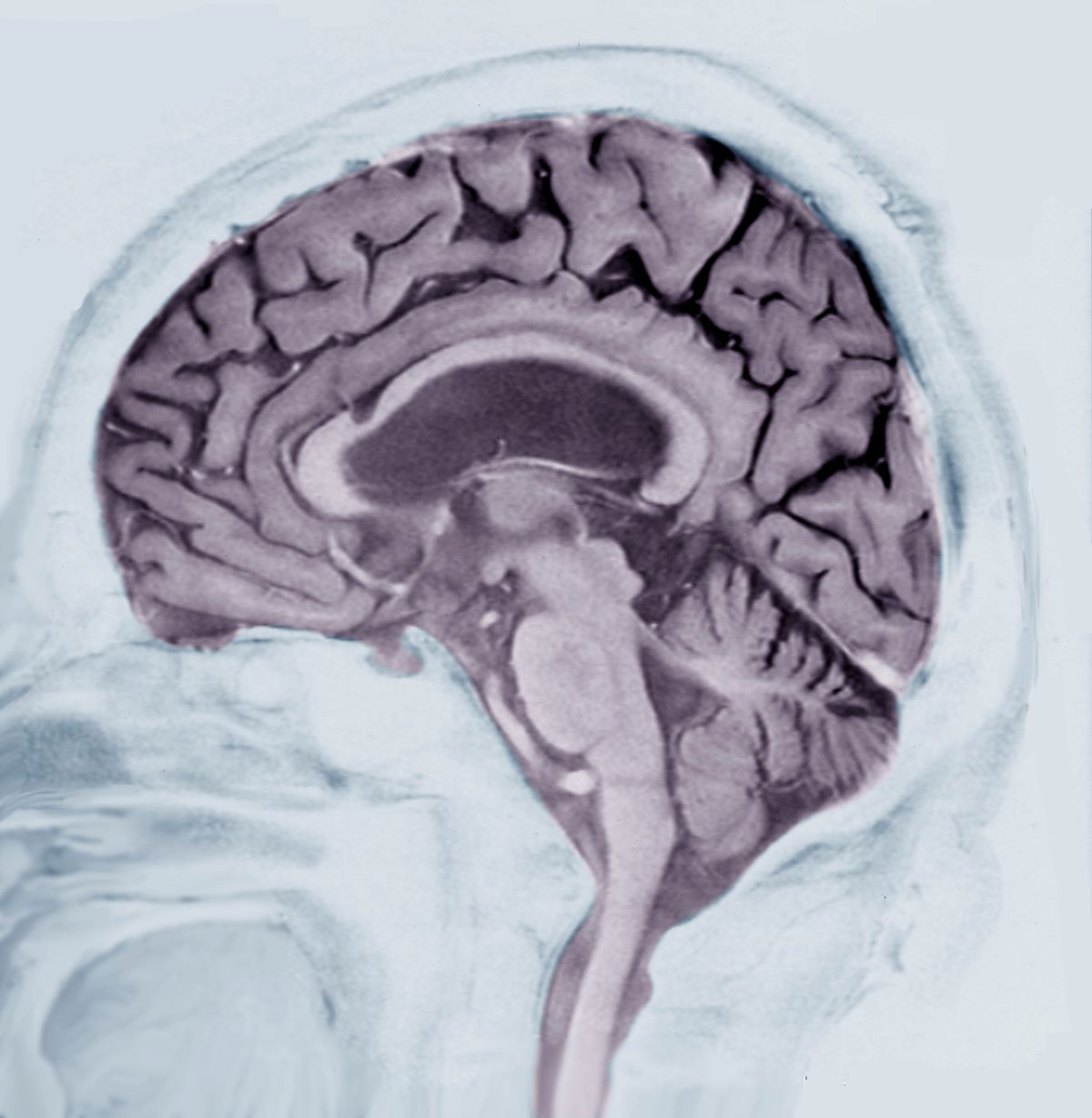
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 52-year-old female presents complaining of fatigue, brain fog, and headaches. She reports that, over the last year, she feels increasingly more irritable, anxious, overwhelmed, and sometimes disoriented. When prompted, she admits to having trouble keeping track of things — dates, important deadlines, objects like her keys, and things she uses each day. She needs multiple reminder events or tasks and must write everything down. She also reports that she often loses her train of thought and sometimes struggles to find words. She works in a medical office, is married, and has two children in college. She helps with caring for her in-laws on the weekend by doing their bills and grocery shopping. She admits to being moody and does not want to socialize, which she attributes to fatigue and having a busy life. She also complains of muscle stiffness and general clumsiness. Eight months ago, the patient was in an automobile accident in which her car was totaled, but she did not sustain serious injury and opted not to seek medical evaluation.
Physical exam reveals slight visuospatial dysfunction, with issues with both coordination and balance. The patient appears fatigued and has some trouble maintaining her attention during the conversation. Further questioning reveals mild anomic aphasia and some lapses in recent memory. Her reflexes are otherwise normal, as are heart, lung, and breath sounds. All systemic lymph nodes are normal as are liver and spleen on palpation. The patient recently discovered that her estranged father had been diagnosed with Alzheimer’s disease (AD) at 58 years of age and passed away 5 years later.
Laboratory testing is performed and reveals nothing remarkable. Considering the car accident and new cognitive/behavioral changes experienced by the patient, a CT of the brain is ordered. Results are negative for concussion and cerebral hemorrhage but show cortical atrophy of the temporal territories and a large increase in the size of the subarachnoid spaces predominantly affecting the parietal region.
Alzheimer's Disease and Athletes
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Progressive cognitive decline
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
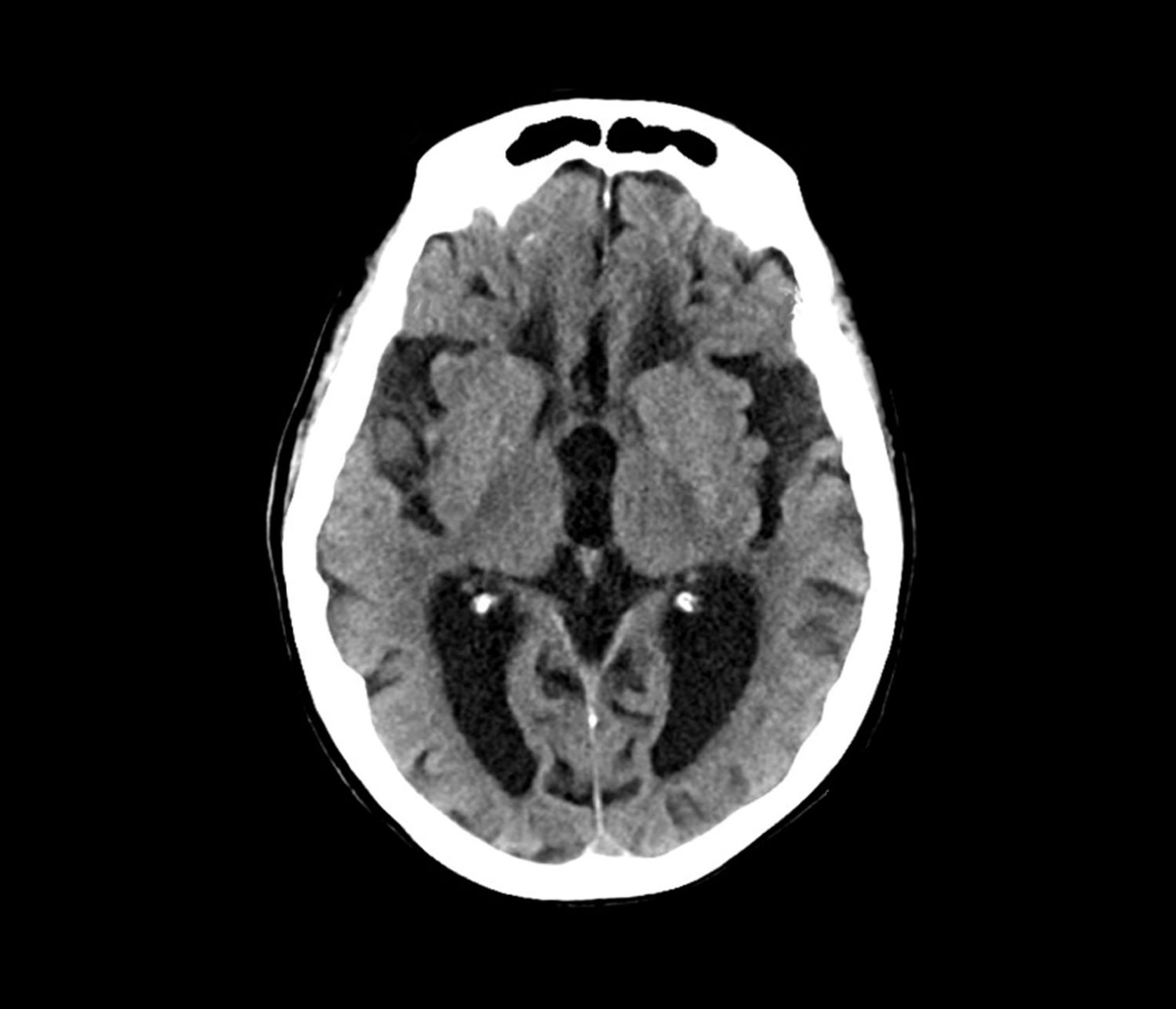
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 40-year-old man with Down syndrome (DS) presented with progressive cognitive decline over 2 years, characterized by memory impairment, difficulty performing familiar tasks, and increasing disorientation. His caregivers noted mood changes, including irritability and withdrawal, and occasional episodes of agitation. Clinical history revealed congenital heart disease (surgically repaired in childhood) and hypothyroidism, which was well controlled with levothyroxine. Physical examination showed no focal neurologic deficits, but he exhibited mild hypotonia, a characteristic feature of DS, and a shuffling gait. Routine blood tests revealed normal thyroid function, no evidence of vitamin B12 deficiency, and unremarkable metabolic panels. An MRI scan (as shown in the image) demonstrated marked ventricular enlargement and generalized cortical atrophy.
Alzheimer's Disease & Down Syndrome
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Updated Alzheimer’s Guidelines Chart the Full Diagnostic Journey
This is the first update since 2001 for specialists and the first guideline for primary care physicians. Executive summaries of the guidelines were published in three articles online on December 23 in a special issue of Alzheimer’s & Dementia.
What’s New?
“With this guideline, we expand the scope of prior guidelines by providing recommendations for practicing clinicians on the process from start to finish,” coauthor Brad Dickerson, MD, director of the Massachusetts General Hospital Frontotemporal Disorders Unit and professor of neurology at Harvard Medical School, Boston, said in a statement.
“If clinicians adopt these recommendations and healthcare systems provide adequate resources, outcomes should improve in most patients in most practice settings,” Dickerson added in an interview.
Through a modified-Delphi approach and guideline-development process, an expert workgroup representing primary and specialty care reviewed 7374 publications, of which 133 met inclusion criteria.
Based on the information, the workgroup outlined a three-step patient-centered evaluation process, which includes assessing cognitive functional status, identifying the cognitive-behavioral syndrome based on specific symptoms, and determining the likely brain diseases or conditions causing the symptoms.
What Are the Key Recommendations?
The guidelines include 19 “practical” recommendations that are applicable to any practice setting. They capture the core elements of a high-quality evaluation and disclosure process, the author said. Here is a brief summary of the recommendations:
Initial evaluation: Perform a multitiered evaluation for patients who self-report or whose care partner or clinician reports cognitive, behavioral, or functional changes.
Patient-centered communication: Partner with the patient and/or care partner to establish shared goals for the evaluation process; assess the patient’s capacity to engage in goal setting.
Diagnostic formulation: Use a tiered approach to assessments and tests based on individual presentation, risk factors, and profile, aiming to determine the level of impairment, cognitive-behavioral syndrome, and likely causes and contributing factors.
History taking: Gather reliable information from informants about changes in cognition, activities of daily living, mood, neuropsychiatric symptoms, and sensory/motor functions. Document individualized risk factors for cognitive decline.
Examination: Conduct a comprehensive examination of cognition, mood, behavior, and a dementia-focused neurologic evaluation using validated tools.
Laboratory tests: Perform tiered, individualized laboratory evaluations, starting with routine tests for all patients.
Structural imaging: Obtain structural brain imaging (MRI preferred, CT as an alternative) to help establish a cause.
Ongoing communication: Engage in ongoing dialogue with patient/care partner to guide them throughout the diagnostic process.
Diagnostic disclosure: Share findings honestly and compassionately, explaining the syndrome, its severity, probable cause, prognosis, treatment options and support resources.
Specialist referral: Refer patients with atypical, uncertain, early-onset, or rapidly progressing symptoms to a dementia subspecialist.
Neuropsychological testing: Use in instances of diagnostic uncertainty or patients with complex clinical profiles. At a minimum, the neuropsychological evaluation should include normed neuropsychological testing of the domains of learning and memory (in particular delayed free and cued recall/recognition), attention, executive function, visuospatial function, and language.
Advanced diagnostic testing: When diagnostic uncertainty remains, obtain additional laboratory tests tailored to individual patient profiles.
Molecular imaging: In a patient with an established cognitive-behavioral syndrome in whom there is continued diagnostic uncertainty regarding cause(s) after structural imaging, a dementia specialist can obtain molecular imaging with fluorodeoxyglucose PET to improve diagnostic accuracy.
Cerebrospinal fluid (CSF) analysis: Utilize CSF biomarkers to evaluate amyloid beta and tau profiles in cases with unresolved diagnostic uncertainty.
Amyloid PET imaging: Perform amyloid PET scans for patients with persistent diagnostic uncertainty after other assessments.
Genetic counseling and testing: Consider genetic testing for patients with strong autosomal dominant family histories and involve a genetic counselor.
Future Directions?
Maria C. Carrillo, PhD, chief science officer and medical affairs lead for the Alzheimer’s Association, encourages clinicians to incorporate these guidelines into their practice.
“These guidelines are important because they guide clinicians in the evaluation of memory complaints, which could have many underlying causes. That is the necessary start for an early and accurate Alzheimer’s diagnosis,” Carrillo said in a statement.
Dickerson said the new guidelines do not address blood-based biomarkers “because nobody really feels that they are ready for prime time yet, even though they’re getting rolled out as clinical products.”
However, the recommendations will be revised as needed. “That’s one of the values of setting this up as a process; whenever any new development occurs, it will be easy to update the guidelines to show where that new test or new biomarker fits in the overall process,” he said.
New Appropriate Use Guidance
A separate workgroup, jointly convened by the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging, has revised appropriate use criteria (AUC) for amyloid PET imaging and developed AUC for tau PET imaging.
They were simultaneously published online in Alzheimer’s & Dementia and The Journal of Nuclear Medicine. They are the first revision since the initial AUC for amyloid PET was introduced in 2013.
“The updated amyloid/tau appropriate use criteria will help ensure these tracers are used in a cost-effective manner and the scan results will be used appropriately to add value to the diagnosis and management of dementia,” said workgroup members Kevin Donohoe, MD, with Beth Israel Deaconess Medical Center, Boston, and Phillip Kuo, MD, with City of Hope National Medical Center, Duarte, California.
The AUC include 17 real-world scenarios in which amyloid or tau PET may be considered, with the two tests considered separately and given their own rating for each scenario.
Overall, the strongest evidence for their use includes assessment and prognosis for people with mild cognitive impairment; assessment of people with dementia when the cause is not clearly known; and determining eligibility for treatment with new disease-modifying therapies, and monitoring response to these treatments, the workgroup said.
“Whereas the prior AUC was written at a time when only the deposition of amyloid could be documented, the new therapeutic agents allow us to demonstrate the actual clearance of amyloid during therapy,” Donohoe and Kuo explained.
“These new therapeutic agents are expensive and, as with most medications, may cause unwanted side effects. The most recent version of the AUC includes information about the appropriate use of amyloid imaging for both documenting the presence of amyloid deposits in the brain, making anti-amyloid therapy an option, as well as documenting the effectiveness of the therapeutic agents as amyloid is (or is not) cleared from the brain,” Donahoe and Kuo noted.
The revised AUC also state that, in most cases, amyloid and tau PET tests should not be used for people who do not have cognitive impairment, even if they carry the APOE4 risk-related gene for Alzheimer’s disease; nonmedical use such as for legal concerns, insurance coverage, or employment screening; and in place of genetic testing in patients suspected of carrying a disease-causing genetic mutation.
In a statement, lead author Gil D. Rabinovici, MD, with University of California, San Francisco, emphasized that the AUC “should be considered guidelines for clinicians, not a substitute for careful clinical judgment that considers the full clinical context for each patient with cognitive complaints.”
This research was funded by the Alzheimer’s Association. Disclosures for guideline authors are available with the original articles.
A version of this article first appeared on Medscape.com.
This is the first update since 2001 for specialists and the first guideline for primary care physicians. Executive summaries of the guidelines were published in three articles online on December 23 in a special issue of Alzheimer’s & Dementia.
What’s New?
“With this guideline, we expand the scope of prior guidelines by providing recommendations for practicing clinicians on the process from start to finish,” coauthor Brad Dickerson, MD, director of the Massachusetts General Hospital Frontotemporal Disorders Unit and professor of neurology at Harvard Medical School, Boston, said in a statement.
“If clinicians adopt these recommendations and healthcare systems provide adequate resources, outcomes should improve in most patients in most practice settings,” Dickerson added in an interview.
Through a modified-Delphi approach and guideline-development process, an expert workgroup representing primary and specialty care reviewed 7374 publications, of which 133 met inclusion criteria.
Based on the information, the workgroup outlined a three-step patient-centered evaluation process, which includes assessing cognitive functional status, identifying the cognitive-behavioral syndrome based on specific symptoms, and determining the likely brain diseases or conditions causing the symptoms.
What Are the Key Recommendations?
The guidelines include 19 “practical” recommendations that are applicable to any practice setting. They capture the core elements of a high-quality evaluation and disclosure process, the author said. Here is a brief summary of the recommendations:
Initial evaluation: Perform a multitiered evaluation for patients who self-report or whose care partner or clinician reports cognitive, behavioral, or functional changes.
Patient-centered communication: Partner with the patient and/or care partner to establish shared goals for the evaluation process; assess the patient’s capacity to engage in goal setting.
Diagnostic formulation: Use a tiered approach to assessments and tests based on individual presentation, risk factors, and profile, aiming to determine the level of impairment, cognitive-behavioral syndrome, and likely causes and contributing factors.
History taking: Gather reliable information from informants about changes in cognition, activities of daily living, mood, neuropsychiatric symptoms, and sensory/motor functions. Document individualized risk factors for cognitive decline.
Examination: Conduct a comprehensive examination of cognition, mood, behavior, and a dementia-focused neurologic evaluation using validated tools.
Laboratory tests: Perform tiered, individualized laboratory evaluations, starting with routine tests for all patients.
Structural imaging: Obtain structural brain imaging (MRI preferred, CT as an alternative) to help establish a cause.
Ongoing communication: Engage in ongoing dialogue with patient/care partner to guide them throughout the diagnostic process.
Diagnostic disclosure: Share findings honestly and compassionately, explaining the syndrome, its severity, probable cause, prognosis, treatment options and support resources.
Specialist referral: Refer patients with atypical, uncertain, early-onset, or rapidly progressing symptoms to a dementia subspecialist.
Neuropsychological testing: Use in instances of diagnostic uncertainty or patients with complex clinical profiles. At a minimum, the neuropsychological evaluation should include normed neuropsychological testing of the domains of learning and memory (in particular delayed free and cued recall/recognition), attention, executive function, visuospatial function, and language.
Advanced diagnostic testing: When diagnostic uncertainty remains, obtain additional laboratory tests tailored to individual patient profiles.
Molecular imaging: In a patient with an established cognitive-behavioral syndrome in whom there is continued diagnostic uncertainty regarding cause(s) after structural imaging, a dementia specialist can obtain molecular imaging with fluorodeoxyglucose PET to improve diagnostic accuracy.
Cerebrospinal fluid (CSF) analysis: Utilize CSF biomarkers to evaluate amyloid beta and tau profiles in cases with unresolved diagnostic uncertainty.
Amyloid PET imaging: Perform amyloid PET scans for patients with persistent diagnostic uncertainty after other assessments.
Genetic counseling and testing: Consider genetic testing for patients with strong autosomal dominant family histories and involve a genetic counselor.
Future Directions?
Maria C. Carrillo, PhD, chief science officer and medical affairs lead for the Alzheimer’s Association, encourages clinicians to incorporate these guidelines into their practice.
“These guidelines are important because they guide clinicians in the evaluation of memory complaints, which could have many underlying causes. That is the necessary start for an early and accurate Alzheimer’s diagnosis,” Carrillo said in a statement.
Dickerson said the new guidelines do not address blood-based biomarkers “because nobody really feels that they are ready for prime time yet, even though they’re getting rolled out as clinical products.”
However, the recommendations will be revised as needed. “That’s one of the values of setting this up as a process; whenever any new development occurs, it will be easy to update the guidelines to show where that new test or new biomarker fits in the overall process,” he said.
New Appropriate Use Guidance
A separate workgroup, jointly convened by the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging, has revised appropriate use criteria (AUC) for amyloid PET imaging and developed AUC for tau PET imaging.
They were simultaneously published online in Alzheimer’s & Dementia and The Journal of Nuclear Medicine. They are the first revision since the initial AUC for amyloid PET was introduced in 2013.
“The updated amyloid/tau appropriate use criteria will help ensure these tracers are used in a cost-effective manner and the scan results will be used appropriately to add value to the diagnosis and management of dementia,” said workgroup members Kevin Donohoe, MD, with Beth Israel Deaconess Medical Center, Boston, and Phillip Kuo, MD, with City of Hope National Medical Center, Duarte, California.
The AUC include 17 real-world scenarios in which amyloid or tau PET may be considered, with the two tests considered separately and given their own rating for each scenario.
Overall, the strongest evidence for their use includes assessment and prognosis for people with mild cognitive impairment; assessment of people with dementia when the cause is not clearly known; and determining eligibility for treatment with new disease-modifying therapies, and monitoring response to these treatments, the workgroup said.
“Whereas the prior AUC was written at a time when only the deposition of amyloid could be documented, the new therapeutic agents allow us to demonstrate the actual clearance of amyloid during therapy,” Donohoe and Kuo explained.
“These new therapeutic agents are expensive and, as with most medications, may cause unwanted side effects. The most recent version of the AUC includes information about the appropriate use of amyloid imaging for both documenting the presence of amyloid deposits in the brain, making anti-amyloid therapy an option, as well as documenting the effectiveness of the therapeutic agents as amyloid is (or is not) cleared from the brain,” Donahoe and Kuo noted.
The revised AUC also state that, in most cases, amyloid and tau PET tests should not be used for people who do not have cognitive impairment, even if they carry the APOE4 risk-related gene for Alzheimer’s disease; nonmedical use such as for legal concerns, insurance coverage, or employment screening; and in place of genetic testing in patients suspected of carrying a disease-causing genetic mutation.
In a statement, lead author Gil D. Rabinovici, MD, with University of California, San Francisco, emphasized that the AUC “should be considered guidelines for clinicians, not a substitute for careful clinical judgment that considers the full clinical context for each patient with cognitive complaints.”
This research was funded by the Alzheimer’s Association. Disclosures for guideline authors are available with the original articles.
A version of this article first appeared on Medscape.com.
This is the first update since 2001 for specialists and the first guideline for primary care physicians. Executive summaries of the guidelines were published in three articles online on December 23 in a special issue of Alzheimer’s & Dementia.
What’s New?
“With this guideline, we expand the scope of prior guidelines by providing recommendations for practicing clinicians on the process from start to finish,” coauthor Brad Dickerson, MD, director of the Massachusetts General Hospital Frontotemporal Disorders Unit and professor of neurology at Harvard Medical School, Boston, said in a statement.
“If clinicians adopt these recommendations and healthcare systems provide adequate resources, outcomes should improve in most patients in most practice settings,” Dickerson added in an interview.
Through a modified-Delphi approach and guideline-development process, an expert workgroup representing primary and specialty care reviewed 7374 publications, of which 133 met inclusion criteria.
Based on the information, the workgroup outlined a three-step patient-centered evaluation process, which includes assessing cognitive functional status, identifying the cognitive-behavioral syndrome based on specific symptoms, and determining the likely brain diseases or conditions causing the symptoms.
What Are the Key Recommendations?
The guidelines include 19 “practical” recommendations that are applicable to any practice setting. They capture the core elements of a high-quality evaluation and disclosure process, the author said. Here is a brief summary of the recommendations:
Initial evaluation: Perform a multitiered evaluation for patients who self-report or whose care partner or clinician reports cognitive, behavioral, or functional changes.
Patient-centered communication: Partner with the patient and/or care partner to establish shared goals for the evaluation process; assess the patient’s capacity to engage in goal setting.
Diagnostic formulation: Use a tiered approach to assessments and tests based on individual presentation, risk factors, and profile, aiming to determine the level of impairment, cognitive-behavioral syndrome, and likely causes and contributing factors.
History taking: Gather reliable information from informants about changes in cognition, activities of daily living, mood, neuropsychiatric symptoms, and sensory/motor functions. Document individualized risk factors for cognitive decline.
Examination: Conduct a comprehensive examination of cognition, mood, behavior, and a dementia-focused neurologic evaluation using validated tools.
Laboratory tests: Perform tiered, individualized laboratory evaluations, starting with routine tests for all patients.
Structural imaging: Obtain structural brain imaging (MRI preferred, CT as an alternative) to help establish a cause.
Ongoing communication: Engage in ongoing dialogue with patient/care partner to guide them throughout the diagnostic process.
Diagnostic disclosure: Share findings honestly and compassionately, explaining the syndrome, its severity, probable cause, prognosis, treatment options and support resources.
Specialist referral: Refer patients with atypical, uncertain, early-onset, or rapidly progressing symptoms to a dementia subspecialist.
Neuropsychological testing: Use in instances of diagnostic uncertainty or patients with complex clinical profiles. At a minimum, the neuropsychological evaluation should include normed neuropsychological testing of the domains of learning and memory (in particular delayed free and cued recall/recognition), attention, executive function, visuospatial function, and language.
Advanced diagnostic testing: When diagnostic uncertainty remains, obtain additional laboratory tests tailored to individual patient profiles.
Molecular imaging: In a patient with an established cognitive-behavioral syndrome in whom there is continued diagnostic uncertainty regarding cause(s) after structural imaging, a dementia specialist can obtain molecular imaging with fluorodeoxyglucose PET to improve diagnostic accuracy.
Cerebrospinal fluid (CSF) analysis: Utilize CSF biomarkers to evaluate amyloid beta and tau profiles in cases with unresolved diagnostic uncertainty.
Amyloid PET imaging: Perform amyloid PET scans for patients with persistent diagnostic uncertainty after other assessments.
Genetic counseling and testing: Consider genetic testing for patients with strong autosomal dominant family histories and involve a genetic counselor.
Future Directions?
Maria C. Carrillo, PhD, chief science officer and medical affairs lead for the Alzheimer’s Association, encourages clinicians to incorporate these guidelines into their practice.
“These guidelines are important because they guide clinicians in the evaluation of memory complaints, which could have many underlying causes. That is the necessary start for an early and accurate Alzheimer’s diagnosis,” Carrillo said in a statement.
Dickerson said the new guidelines do not address blood-based biomarkers “because nobody really feels that they are ready for prime time yet, even though they’re getting rolled out as clinical products.”
However, the recommendations will be revised as needed. “That’s one of the values of setting this up as a process; whenever any new development occurs, it will be easy to update the guidelines to show where that new test or new biomarker fits in the overall process,” he said.
New Appropriate Use Guidance
A separate workgroup, jointly convened by the Alzheimer’s Association and the Society of Nuclear Medicine and Molecular Imaging, has revised appropriate use criteria (AUC) for amyloid PET imaging and developed AUC for tau PET imaging.
They were simultaneously published online in Alzheimer’s & Dementia and The Journal of Nuclear Medicine. They are the first revision since the initial AUC for amyloid PET was introduced in 2013.
“The updated amyloid/tau appropriate use criteria will help ensure these tracers are used in a cost-effective manner and the scan results will be used appropriately to add value to the diagnosis and management of dementia,” said workgroup members Kevin Donohoe, MD, with Beth Israel Deaconess Medical Center, Boston, and Phillip Kuo, MD, with City of Hope National Medical Center, Duarte, California.
The AUC include 17 real-world scenarios in which amyloid or tau PET may be considered, with the two tests considered separately and given their own rating for each scenario.
Overall, the strongest evidence for their use includes assessment and prognosis for people with mild cognitive impairment; assessment of people with dementia when the cause is not clearly known; and determining eligibility for treatment with new disease-modifying therapies, and monitoring response to these treatments, the workgroup said.
“Whereas the prior AUC was written at a time when only the deposition of amyloid could be documented, the new therapeutic agents allow us to demonstrate the actual clearance of amyloid during therapy,” Donohoe and Kuo explained.
“These new therapeutic agents are expensive and, as with most medications, may cause unwanted side effects. The most recent version of the AUC includes information about the appropriate use of amyloid imaging for both documenting the presence of amyloid deposits in the brain, making anti-amyloid therapy an option, as well as documenting the effectiveness of the therapeutic agents as amyloid is (or is not) cleared from the brain,” Donahoe and Kuo noted.
The revised AUC also state that, in most cases, amyloid and tau PET tests should not be used for people who do not have cognitive impairment, even if they carry the APOE4 risk-related gene for Alzheimer’s disease; nonmedical use such as for legal concerns, insurance coverage, or employment screening; and in place of genetic testing in patients suspected of carrying a disease-causing genetic mutation.
In a statement, lead author Gil D. Rabinovici, MD, with University of California, San Francisco, emphasized that the AUC “should be considered guidelines for clinicians, not a substitute for careful clinical judgment that considers the full clinical context for each patient with cognitive complaints.”
This research was funded by the Alzheimer’s Association. Disclosures for guideline authors are available with the original articles.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S & DEMENTIA
Losing Your Mind Trying to Understand the BP-Dementia Link
You could be forgiven if you are confused about how blood pressure (BP) affects dementia. First, you read an article extolling the benefits of BP lowering, then a study about how stopping antihypertensives slows cognitive decline in nursing home residents. It’s enough to make you lose your mind.
The Brain Benefits of BP Lowering
It should be stated unequivocally that you should absolutely treat high BP. It may have once been acceptable to state, “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.” But those dark days are long behind us.
In these divided times, at least we can agree that we should treat high BP. The cardiovascular (CV) benefits, in and of themselves, justify the decision. But BP’s relationship with dementia is more complex. There are different types of dementia even though we tend to lump them all into one category. Vascular dementia is driven by the same pathophysiology and risk factors as cardiac disease. It’s intuitive that treating hypertension, diabetes, hypercholesterolemia, and smoking will decrease the risk for stroke and limit the damage to the brain that we see with repeated vascular insults. For Alzheimer’s disease, high BP and other CV risk factors seem to increase the risk even if the mechanism is not fully elucidated.
Estimates suggest that if we could lower the prevalence of hypertension by 25%, there would be 160,000 fewer cases of Alzheimer’s disease. But the data are not as robust as one might hope. A 2021 Cochrane review found that hypertension treatment slowed cognitive decline, but the quality of the evidence was low. Short duration of follow-up, dropouts, crossovers, and other problems with the data precluded any certainty. What’s more, hypertension in midlife is associated with cognitive decline and dementia, but its impact in those over age 70 is less clear. Later in life, or once cognitive impairment has already developed, it may be too late for BP lowering to have any impact.
Potential Harms of Lowering BP
All this needs to be weighed against the potential harms of treating hypertension. I will reiterate that hypertension should be treated and treated aggressively for the prevention of CV events. But overtreatment, especially in older patients, is associated with hypotension, falls, and syncope. Older patients are also at risk for polypharmacy and drug-drug interactions.
A Korean nationwide survey showed a U-shaped association between BP and Alzheimer’s disease risk in adults (mean age, 67 years), with both high and low BPs associated with a higher risk for Alzheimer’s disease. Though not all studies agree. A post hoc analysis of SPRINT MIND did not find any negative impact of intensive BP lowering on cognitive outcomes or cerebral perfusion in older adults (mean age, 68 years). But it didn’t do much good either. Given the heterogeneity of the data, doubts remain on whether aggressive BP lowering might be detrimental in older patients with comorbidities and preexisting dementia. The obvious corollary then is whether deprescribing hypertensive medications could be beneficial.
A recent publication in JAMA Internal Medicine attempted to address this very question. The cohort study used data from Veterans Affairs nursing home residents (mean age, 78 years) to emulate a randomized trial on deprescribing antihypertensives and cognitive decline. Many of the residents’ cognitive scores worsened over the course of follow-up; however, the decline was less pronounced in the deprescribing group (10% vs 12%). The same group did a similar analysis looking at CV outcomes and found no increased risk for heart attack or stroke with deprescribing BP medications. Taken together, these nursing home data suggest that deprescribing may help slow cognitive decline without the expected trade-off of increased CV events.
Deprescribing, Yes or No?
However, randomized data would obviously be preferable, and these are in short supply. One such trial, the DANTE study, found no benefit to deprescribing in terms of cognition in adults aged 75 years or older with mild cognitive impairment. The study follow-up was only 16 weeks, however, which is hardly enough time to demonstrate any effect, positive or negative. The most that can be said is that it didn’t cause many short-term adverse events.
Perhaps the best conclusion to draw from this somewhat underwhelming collection of data is that lowering high BP is important, but less important the closer we get to the end of life. Hypotension is obviously bad, and overly aggressive BP lowering is going to lead to negative outcomes in older adults because gravity is an unforgiving mistress.
Deprescribing antihypertensives in older adults is probably not going to cause major negative outcomes, but whether it will do much good in nonhypotensive patients is debatable. The bigger problem is the millions of people with undiagnosed or undertreated hypertension. We would probably have less dementia if we treated hypertension when it does the most good: as a primary-prevention strategy in midlife.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, Quebec, Canada. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
You could be forgiven if you are confused about how blood pressure (BP) affects dementia. First, you read an article extolling the benefits of BP lowering, then a study about how stopping antihypertensives slows cognitive decline in nursing home residents. It’s enough to make you lose your mind.
The Brain Benefits of BP Lowering
It should be stated unequivocally that you should absolutely treat high BP. It may have once been acceptable to state, “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.” But those dark days are long behind us.
In these divided times, at least we can agree that we should treat high BP. The cardiovascular (CV) benefits, in and of themselves, justify the decision. But BP’s relationship with dementia is more complex. There are different types of dementia even though we tend to lump them all into one category. Vascular dementia is driven by the same pathophysiology and risk factors as cardiac disease. It’s intuitive that treating hypertension, diabetes, hypercholesterolemia, and smoking will decrease the risk for stroke and limit the damage to the brain that we see with repeated vascular insults. For Alzheimer’s disease, high BP and other CV risk factors seem to increase the risk even if the mechanism is not fully elucidated.
Estimates suggest that if we could lower the prevalence of hypertension by 25%, there would be 160,000 fewer cases of Alzheimer’s disease. But the data are not as robust as one might hope. A 2021 Cochrane review found that hypertension treatment slowed cognitive decline, but the quality of the evidence was low. Short duration of follow-up, dropouts, crossovers, and other problems with the data precluded any certainty. What’s more, hypertension in midlife is associated with cognitive decline and dementia, but its impact in those over age 70 is less clear. Later in life, or once cognitive impairment has already developed, it may be too late for BP lowering to have any impact.
Potential Harms of Lowering BP
All this needs to be weighed against the potential harms of treating hypertension. I will reiterate that hypertension should be treated and treated aggressively for the prevention of CV events. But overtreatment, especially in older patients, is associated with hypotension, falls, and syncope. Older patients are also at risk for polypharmacy and drug-drug interactions.
A Korean nationwide survey showed a U-shaped association between BP and Alzheimer’s disease risk in adults (mean age, 67 years), with both high and low BPs associated with a higher risk for Alzheimer’s disease. Though not all studies agree. A post hoc analysis of SPRINT MIND did not find any negative impact of intensive BP lowering on cognitive outcomes or cerebral perfusion in older adults (mean age, 68 years). But it didn’t do much good either. Given the heterogeneity of the data, doubts remain on whether aggressive BP lowering might be detrimental in older patients with comorbidities and preexisting dementia. The obvious corollary then is whether deprescribing hypertensive medications could be beneficial.
A recent publication in JAMA Internal Medicine attempted to address this very question. The cohort study used data from Veterans Affairs nursing home residents (mean age, 78 years) to emulate a randomized trial on deprescribing antihypertensives and cognitive decline. Many of the residents’ cognitive scores worsened over the course of follow-up; however, the decline was less pronounced in the deprescribing group (10% vs 12%). The same group did a similar analysis looking at CV outcomes and found no increased risk for heart attack or stroke with deprescribing BP medications. Taken together, these nursing home data suggest that deprescribing may help slow cognitive decline without the expected trade-off of increased CV events.
Deprescribing, Yes or No?
However, randomized data would obviously be preferable, and these are in short supply. One such trial, the DANTE study, found no benefit to deprescribing in terms of cognition in adults aged 75 years or older with mild cognitive impairment. The study follow-up was only 16 weeks, however, which is hardly enough time to demonstrate any effect, positive or negative. The most that can be said is that it didn’t cause many short-term adverse events.
Perhaps the best conclusion to draw from this somewhat underwhelming collection of data is that lowering high BP is important, but less important the closer we get to the end of life. Hypotension is obviously bad, and overly aggressive BP lowering is going to lead to negative outcomes in older adults because gravity is an unforgiving mistress.
Deprescribing antihypertensives in older adults is probably not going to cause major negative outcomes, but whether it will do much good in nonhypotensive patients is debatable. The bigger problem is the millions of people with undiagnosed or undertreated hypertension. We would probably have less dementia if we treated hypertension when it does the most good: as a primary-prevention strategy in midlife.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, Quebec, Canada. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
You could be forgiven if you are confused about how blood pressure (BP) affects dementia. First, you read an article extolling the benefits of BP lowering, then a study about how stopping antihypertensives slows cognitive decline in nursing home residents. It’s enough to make you lose your mind.
The Brain Benefits of BP Lowering
It should be stated unequivocally that you should absolutely treat high BP. It may have once been acceptable to state, “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.” But those dark days are long behind us.
In these divided times, at least we can agree that we should treat high BP. The cardiovascular (CV) benefits, in and of themselves, justify the decision. But BP’s relationship with dementia is more complex. There are different types of dementia even though we tend to lump them all into one category. Vascular dementia is driven by the same pathophysiology and risk factors as cardiac disease. It’s intuitive that treating hypertension, diabetes, hypercholesterolemia, and smoking will decrease the risk for stroke and limit the damage to the brain that we see with repeated vascular insults. For Alzheimer’s disease, high BP and other CV risk factors seem to increase the risk even if the mechanism is not fully elucidated.
Estimates suggest that if we could lower the prevalence of hypertension by 25%, there would be 160,000 fewer cases of Alzheimer’s disease. But the data are not as robust as one might hope. A 2021 Cochrane review found that hypertension treatment slowed cognitive decline, but the quality of the evidence was low. Short duration of follow-up, dropouts, crossovers, and other problems with the data precluded any certainty. What’s more, hypertension in midlife is associated with cognitive decline and dementia, but its impact in those over age 70 is less clear. Later in life, or once cognitive impairment has already developed, it may be too late for BP lowering to have any impact.
Potential Harms of Lowering BP
All this needs to be weighed against the potential harms of treating hypertension. I will reiterate that hypertension should be treated and treated aggressively for the prevention of CV events. But overtreatment, especially in older patients, is associated with hypotension, falls, and syncope. Older patients are also at risk for polypharmacy and drug-drug interactions.
A Korean nationwide survey showed a U-shaped association between BP and Alzheimer’s disease risk in adults (mean age, 67 years), with both high and low BPs associated with a higher risk for Alzheimer’s disease. Though not all studies agree. A post hoc analysis of SPRINT MIND did not find any negative impact of intensive BP lowering on cognitive outcomes or cerebral perfusion in older adults (mean age, 68 years). But it didn’t do much good either. Given the heterogeneity of the data, doubts remain on whether aggressive BP lowering might be detrimental in older patients with comorbidities and preexisting dementia. The obvious corollary then is whether deprescribing hypertensive medications could be beneficial.
A recent publication in JAMA Internal Medicine attempted to address this very question. The cohort study used data from Veterans Affairs nursing home residents (mean age, 78 years) to emulate a randomized trial on deprescribing antihypertensives and cognitive decline. Many of the residents’ cognitive scores worsened over the course of follow-up; however, the decline was less pronounced in the deprescribing group (10% vs 12%). The same group did a similar analysis looking at CV outcomes and found no increased risk for heart attack or stroke with deprescribing BP medications. Taken together, these nursing home data suggest that deprescribing may help slow cognitive decline without the expected trade-off of increased CV events.
Deprescribing, Yes or No?
However, randomized data would obviously be preferable, and these are in short supply. One such trial, the DANTE study, found no benefit to deprescribing in terms of cognition in adults aged 75 years or older with mild cognitive impairment. The study follow-up was only 16 weeks, however, which is hardly enough time to demonstrate any effect, positive or negative. The most that can be said is that it didn’t cause many short-term adverse events.
Perhaps the best conclusion to draw from this somewhat underwhelming collection of data is that lowering high BP is important, but less important the closer we get to the end of life. Hypotension is obviously bad, and overly aggressive BP lowering is going to lead to negative outcomes in older adults because gravity is an unforgiving mistress.
Deprescribing antihypertensives in older adults is probably not going to cause major negative outcomes, but whether it will do much good in nonhypotensive patients is debatable. The bigger problem is the millions of people with undiagnosed or undertreated hypertension. We would probably have less dementia if we treated hypertension when it does the most good: as a primary-prevention strategy in midlife.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, Quebec, Canada. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Early-Onset Asthma May Slow Memory Development
Children with asthma scored significantly lower than those without asthma on measures of episodic memory, based on longitudinal data from nearly 500 individuals.
Animal models have shown associations between asthma and memory problems, but data for children are lacking, wrote Nicholas J. Christopher-Hayes, MA, of the University of California, Davis, and colleagues.
“Asthma is very frequent among children, and there is mounting evidence from rodent models that asthma may result in neural injury in the hippocampus, which in turn may cause memory loss,” Christopher-Hayes said in an interview. “Although there is also a good amount of research with older adults, very little research has been done with children, the period that is most frequently linked to asthma onset,” he said. Therefore, the researchers leveraged a large national study on child development to examine development of memory as a function of asthma exposure.
In this study published in JAMA Network Open, the researchers conducted both a longitudinal and cross-sectional analysis of data from the Adolescent Brain Cognitive Development Study, which began in 2015. Children were enrolled at ages 9-10 years with a follow-up assessment 1-2 years later.
The participants were categorized as early childhood-onset asthma (asthma at baseline and follow-up), later childhood-onset asthma (asthma at follow-up only), or no asthma history. The primary outcome of the longitudinal analysis was episodic memory. Approximately half of the participants were boys, and slightly more than half were White.
Overall, those with early-onset asthma showed significantly lower rates of longitudinal memory improvements at follow-up compared with the comparison group (P < .01).
Developmental memory improvement in children with later-onset asthma was not significantly different from the control individuals.
Secondary outcomes included processing speed and inhibition, and attention. In a cross-sectional analysis with a larger sample of 2062 children from the same database (1031 with any asthma), those with asthma scored significantly lower on measures not only of episodic memory but also processing speed and inhibition/attention than children with no asthma, with P values of .04, .01, and .02, respectively.
The results were limited by several factors, including the reliance on parent reports for indicators of asthma and the lack of data on the potential effect of prescription corticosteroid use on neurocognitive development, the researchers noted.
The mechanism behind the association remains unclear; the inflammation associated with asthma may disrupt neural processing and manifest as cognitive dysfunction, as has been seen in rodent models of asthma, the researchers wrote. “It is possible that associations between asthma and developmental trajectories emerge earlier for memory, perhaps due to its sensitivity to subtle hippocampal injury,” they noted.
Longer follow-up studies are needed to fully understand how childhood asthma predicts memory declines or difficulties in childhood and beyond, said Christopher-Hayes. “We also need additional studies to understand why children who were diagnosed earlier and had asthma for longer seem to be particularly affected,” he said.
The results of this study were consistent with previous findings and therefore not surprising, senior author Simona Ghetti, PhD, a professor of psychology at the University of California, Davis, said in an interview. However, the finding that the extent of exposure to asthma was associated with slower memory improvement in childhood was striking, she said. That children with an earlier asthma onset who had disease indicators for a longer period showed a slower development of memory over time, suggests that asthma exposure may affect the developmental trajectory of memory, Ghetti noted.
“Recommendations to clinicians are premature because we need a better understanding of the boundary conditions, such as the minimal level of asthma exposure that might generate memory difficulties,” said Ghetti.
“Nevertheless, our results underscore the importance of looking at asthma as a potential source of cognitive difficulty in children,” she said.
Asthma’s Extensive Effect
Evidence is mounting that a diagnosis of asthma may have implications outside the pulmonary system, Diego J. Maselli, MD, professor and chief of the Division of Pulmonary Diseases & Critical Care at UT Health, San Antonio, said in an interview.
“Asthmatics may be at risk of nasal polyps, allergic rhinitis, and other allergic conditions, but there is emerging of evidence inflammation associated with asthma may affect other organ systems,” said Maselli, who was not involved in the study.
“For example, chronic inflammation in asthmatics may increase the risk of cardiovascular disease,” he said.
Although less is known about the effects of asthma on the nervous system, animal models suggest that inflammation associated with asthma may result in neuronal injury and potential effects on memory, said Maselli.
The findings of this study provide evidence of potential detrimental effects on the memory of children with asthma but should be interpreted with caution, Maselli said. “Children with chronic medical conditions may have an inherent disadvantage compared with their peers due to the burden of their disease, medication utilization and side effects, absenteeism from school, physical limitations, and other disease-specific circumstances,” he noted.
“Uncontrolled asthma, in particular, has strong links to low socioeconomic factors that are closely tied to access to adequate medical care, nutrition, educational institutions, and other relevant contributors to normal cognitive development,” Maselli said. Although the authors account for some of these socioeconomic factors by evaluating income and race, other variables may have influenced the results, he added.
Overall, this study’s findings suggested that the diagnosis of asthma in children may be associated with memory deficits and may influence neurodevelopment; however, more research is needed to determine whether the findings are replicated in other cohorts, said Maselli. “In particular, evaluating the effects of the severity of asthma and different asthma endotypes would be crucial to identify children with a higher risk of memory or cognitive deficits and confirm these associations,” he said.
This study was funded by the Memory and Plasticity Program at the University of California, Davis, and by a Learning, Memory, and Plasticity Training Program Fellowship grant from the National Institutes of Health. The researchers and Maselli had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Children with asthma scored significantly lower than those without asthma on measures of episodic memory, based on longitudinal data from nearly 500 individuals.
Animal models have shown associations between asthma and memory problems, but data for children are lacking, wrote Nicholas J. Christopher-Hayes, MA, of the University of California, Davis, and colleagues.
“Asthma is very frequent among children, and there is mounting evidence from rodent models that asthma may result in neural injury in the hippocampus, which in turn may cause memory loss,” Christopher-Hayes said in an interview. “Although there is also a good amount of research with older adults, very little research has been done with children, the period that is most frequently linked to asthma onset,” he said. Therefore, the researchers leveraged a large national study on child development to examine development of memory as a function of asthma exposure.
In this study published in JAMA Network Open, the researchers conducted both a longitudinal and cross-sectional analysis of data from the Adolescent Brain Cognitive Development Study, which began in 2015. Children were enrolled at ages 9-10 years with a follow-up assessment 1-2 years later.
The participants were categorized as early childhood-onset asthma (asthma at baseline and follow-up), later childhood-onset asthma (asthma at follow-up only), or no asthma history. The primary outcome of the longitudinal analysis was episodic memory. Approximately half of the participants were boys, and slightly more than half were White.
Overall, those with early-onset asthma showed significantly lower rates of longitudinal memory improvements at follow-up compared with the comparison group (P < .01).
Developmental memory improvement in children with later-onset asthma was not significantly different from the control individuals.
Secondary outcomes included processing speed and inhibition, and attention. In a cross-sectional analysis with a larger sample of 2062 children from the same database (1031 with any asthma), those with asthma scored significantly lower on measures not only of episodic memory but also processing speed and inhibition/attention than children with no asthma, with P values of .04, .01, and .02, respectively.
The results were limited by several factors, including the reliance on parent reports for indicators of asthma and the lack of data on the potential effect of prescription corticosteroid use on neurocognitive development, the researchers noted.
The mechanism behind the association remains unclear; the inflammation associated with asthma may disrupt neural processing and manifest as cognitive dysfunction, as has been seen in rodent models of asthma, the researchers wrote. “It is possible that associations between asthma and developmental trajectories emerge earlier for memory, perhaps due to its sensitivity to subtle hippocampal injury,” they noted.
Longer follow-up studies are needed to fully understand how childhood asthma predicts memory declines or difficulties in childhood and beyond, said Christopher-Hayes. “We also need additional studies to understand why children who were diagnosed earlier and had asthma for longer seem to be particularly affected,” he said.
The results of this study were consistent with previous findings and therefore not surprising, senior author Simona Ghetti, PhD, a professor of psychology at the University of California, Davis, said in an interview. However, the finding that the extent of exposure to asthma was associated with slower memory improvement in childhood was striking, she said. That children with an earlier asthma onset who had disease indicators for a longer period showed a slower development of memory over time, suggests that asthma exposure may affect the developmental trajectory of memory, Ghetti noted.
“Recommendations to clinicians are premature because we need a better understanding of the boundary conditions, such as the minimal level of asthma exposure that might generate memory difficulties,” said Ghetti.
“Nevertheless, our results underscore the importance of looking at asthma as a potential source of cognitive difficulty in children,” she said.
Asthma’s Extensive Effect
Evidence is mounting that a diagnosis of asthma may have implications outside the pulmonary system, Diego J. Maselli, MD, professor and chief of the Division of Pulmonary Diseases & Critical Care at UT Health, San Antonio, said in an interview.
“Asthmatics may be at risk of nasal polyps, allergic rhinitis, and other allergic conditions, but there is emerging of evidence inflammation associated with asthma may affect other organ systems,” said Maselli, who was not involved in the study.
“For example, chronic inflammation in asthmatics may increase the risk of cardiovascular disease,” he said.
Although less is known about the effects of asthma on the nervous system, animal models suggest that inflammation associated with asthma may result in neuronal injury and potential effects on memory, said Maselli.
The findings of this study provide evidence of potential detrimental effects on the memory of children with asthma but should be interpreted with caution, Maselli said. “Children with chronic medical conditions may have an inherent disadvantage compared with their peers due to the burden of their disease, medication utilization and side effects, absenteeism from school, physical limitations, and other disease-specific circumstances,” he noted.
“Uncontrolled asthma, in particular, has strong links to low socioeconomic factors that are closely tied to access to adequate medical care, nutrition, educational institutions, and other relevant contributors to normal cognitive development,” Maselli said. Although the authors account for some of these socioeconomic factors by evaluating income and race, other variables may have influenced the results, he added.
Overall, this study’s findings suggested that the diagnosis of asthma in children may be associated with memory deficits and may influence neurodevelopment; however, more research is needed to determine whether the findings are replicated in other cohorts, said Maselli. “In particular, evaluating the effects of the severity of asthma and different asthma endotypes would be crucial to identify children with a higher risk of memory or cognitive deficits and confirm these associations,” he said.
This study was funded by the Memory and Plasticity Program at the University of California, Davis, and by a Learning, Memory, and Plasticity Training Program Fellowship grant from the National Institutes of Health. The researchers and Maselli had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Children with asthma scored significantly lower than those without asthma on measures of episodic memory, based on longitudinal data from nearly 500 individuals.
Animal models have shown associations between asthma and memory problems, but data for children are lacking, wrote Nicholas J. Christopher-Hayes, MA, of the University of California, Davis, and colleagues.
“Asthma is very frequent among children, and there is mounting evidence from rodent models that asthma may result in neural injury in the hippocampus, which in turn may cause memory loss,” Christopher-Hayes said in an interview. “Although there is also a good amount of research with older adults, very little research has been done with children, the period that is most frequently linked to asthma onset,” he said. Therefore, the researchers leveraged a large national study on child development to examine development of memory as a function of asthma exposure.
In this study published in JAMA Network Open, the researchers conducted both a longitudinal and cross-sectional analysis of data from the Adolescent Brain Cognitive Development Study, which began in 2015. Children were enrolled at ages 9-10 years with a follow-up assessment 1-2 years later.
The participants were categorized as early childhood-onset asthma (asthma at baseline and follow-up), later childhood-onset asthma (asthma at follow-up only), or no asthma history. The primary outcome of the longitudinal analysis was episodic memory. Approximately half of the participants were boys, and slightly more than half were White.
Overall, those with early-onset asthma showed significantly lower rates of longitudinal memory improvements at follow-up compared with the comparison group (P < .01).
Developmental memory improvement in children with later-onset asthma was not significantly different from the control individuals.
Secondary outcomes included processing speed and inhibition, and attention. In a cross-sectional analysis with a larger sample of 2062 children from the same database (1031 with any asthma), those with asthma scored significantly lower on measures not only of episodic memory but also processing speed and inhibition/attention than children with no asthma, with P values of .04, .01, and .02, respectively.
The results were limited by several factors, including the reliance on parent reports for indicators of asthma and the lack of data on the potential effect of prescription corticosteroid use on neurocognitive development, the researchers noted.
The mechanism behind the association remains unclear; the inflammation associated with asthma may disrupt neural processing and manifest as cognitive dysfunction, as has been seen in rodent models of asthma, the researchers wrote. “It is possible that associations between asthma and developmental trajectories emerge earlier for memory, perhaps due to its sensitivity to subtle hippocampal injury,” they noted.
Longer follow-up studies are needed to fully understand how childhood asthma predicts memory declines or difficulties in childhood and beyond, said Christopher-Hayes. “We also need additional studies to understand why children who were diagnosed earlier and had asthma for longer seem to be particularly affected,” he said.
The results of this study were consistent with previous findings and therefore not surprising, senior author Simona Ghetti, PhD, a professor of psychology at the University of California, Davis, said in an interview. However, the finding that the extent of exposure to asthma was associated with slower memory improvement in childhood was striking, she said. That children with an earlier asthma onset who had disease indicators for a longer period showed a slower development of memory over time, suggests that asthma exposure may affect the developmental trajectory of memory, Ghetti noted.
“Recommendations to clinicians are premature because we need a better understanding of the boundary conditions, such as the minimal level of asthma exposure that might generate memory difficulties,” said Ghetti.
“Nevertheless, our results underscore the importance of looking at asthma as a potential source of cognitive difficulty in children,” she said.
Asthma’s Extensive Effect
Evidence is mounting that a diagnosis of asthma may have implications outside the pulmonary system, Diego J. Maselli, MD, professor and chief of the Division of Pulmonary Diseases & Critical Care at UT Health, San Antonio, said in an interview.
“Asthmatics may be at risk of nasal polyps, allergic rhinitis, and other allergic conditions, but there is emerging of evidence inflammation associated with asthma may affect other organ systems,” said Maselli, who was not involved in the study.
“For example, chronic inflammation in asthmatics may increase the risk of cardiovascular disease,” he said.
Although less is known about the effects of asthma on the nervous system, animal models suggest that inflammation associated with asthma may result in neuronal injury and potential effects on memory, said Maselli.
The findings of this study provide evidence of potential detrimental effects on the memory of children with asthma but should be interpreted with caution, Maselli said. “Children with chronic medical conditions may have an inherent disadvantage compared with their peers due to the burden of their disease, medication utilization and side effects, absenteeism from school, physical limitations, and other disease-specific circumstances,” he noted.
“Uncontrolled asthma, in particular, has strong links to low socioeconomic factors that are closely tied to access to adequate medical care, nutrition, educational institutions, and other relevant contributors to normal cognitive development,” Maselli said. Although the authors account for some of these socioeconomic factors by evaluating income and race, other variables may have influenced the results, he added.
Overall, this study’s findings suggested that the diagnosis of asthma in children may be associated with memory deficits and may influence neurodevelopment; however, more research is needed to determine whether the findings are replicated in other cohorts, said Maselli. “In particular, evaluating the effects of the severity of asthma and different asthma endotypes would be crucial to identify children with a higher risk of memory or cognitive deficits and confirm these associations,” he said.
This study was funded by the Memory and Plasticity Program at the University of California, Davis, and by a Learning, Memory, and Plasticity Training Program Fellowship grant from the National Institutes of Health. The researchers and Maselli had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Dementia Risk Higher for Stroke Survivors
TOPLINE:
Risk for dementia is nearly 80% higher in stroke survivors than in those without stroke, a new study reveals. The data suggest risk declines within 1 year after stroke but remains elevated for up to 20 years.
METHODOLOGY:
- Researchers conducted a population-wide analysis of over 15 million people in Canada between 2002 and 2022. The study focused on adults hospitalized for ischemic stroke, intracerebral hemorrhage, or acute myocardial infarction (AMI).
- Of 175,980 stroke survivors, 99% were matched 1:1 to residents without stroke on the basis of age, sex, rural residence, neighborhood deprivation, and vascular comorbidities. In addition, 90% of patients were matched to those with AMI.
- Incident dementia diagnoses were tracked starting 90 days after stroke until death, emigration, or the end of the study, using a validated algorithm based on hospitalization for dementia, prescriptions for cholinesterase inhibitors, or physician claims within 2 years.
- The mean follow-up duration was 5.6 years.
TAKEAWAY:
- Among stroke survivors, 19% were diagnosed with dementia vs 12.5% in the reference population. The dementia rate per 100 person-years was higher among stroke survivors than in the reference population over the entire follow-up period (3.34 vs 1.89).
- Over the entire study period, dementia was 76% more likely among stroke patients (hazard ratio [HR], 1.76; 95% CI, 1.73-1.79) and 82% more likely in the AMI cohort (HR, 1.82; 95% CI, 1.79-1.85) than in the reference population.
- Time-varying analysis revealed that dementia risk was highest within the first year after stroke, with a > 2.5-fold increase at 6 months (HR, 2.51; 95% CI, 2.42-2.59), which decreased to a 1.5-fold increase at 5 years (HR, 1.51; 95% CI, 1.48-1.56) but remained elevated compared with the reference population even 20 years after the index stroke.
- Recurrent stroke was associated with an approximately threefold increased risk for dementia (single recurrent stroke adjusted HR, 2.64; 95% CI, 2.54-2.74; multiple recurrent strokes adjusted HR, 3.05; 95% CI, 2.81-3.33).
IN PRACTICE:
“While much research has been focused on reducing the risk of a second stroke, our findings make it clear that more research also is needed on developing interventions to help prevent dementia after stroke,” lead author Raed A. Joundi, MD, DPhil, McMaster University, Hamilton, Ontario, Canada, said in a press release.
“There is a need to accelerate the implementation of promising interventions or multipronged approaches into large randomized controlled trials to lower the risk of dementia,” the investigators wrote.
SOURCE:
The study was published online on December 4 in Neurology.
LIMITATIONS:
The study’s limitations included reliance on administrative coding without imaging data, potential underestimation of mild dementia, and lack of granular information on stroke severity, disability, and prestroke cognitive decline. While adjustments were made for healthcare contact and secondary prevention medications, residual biases may have persisted.
DISCLOSURES:
This study received funding from the Canada Brain Research Fund, Heart & Stroke Foundation of Canada, and Canadian Stroke Consortium. Two authors hold awards and positions from national organizations and academic institutions in Canada. Additional details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Risk for dementia is nearly 80% higher in stroke survivors than in those without stroke, a new study reveals. The data suggest risk declines within 1 year after stroke but remains elevated for up to 20 years.
METHODOLOGY:
- Researchers conducted a population-wide analysis of over 15 million people in Canada between 2002 and 2022. The study focused on adults hospitalized for ischemic stroke, intracerebral hemorrhage, or acute myocardial infarction (AMI).
- Of 175,980 stroke survivors, 99% were matched 1:1 to residents without stroke on the basis of age, sex, rural residence, neighborhood deprivation, and vascular comorbidities. In addition, 90% of patients were matched to those with AMI.
- Incident dementia diagnoses were tracked starting 90 days after stroke until death, emigration, or the end of the study, using a validated algorithm based on hospitalization for dementia, prescriptions for cholinesterase inhibitors, or physician claims within 2 years.
- The mean follow-up duration was 5.6 years.
TAKEAWAY:
- Among stroke survivors, 19% were diagnosed with dementia vs 12.5% in the reference population. The dementia rate per 100 person-years was higher among stroke survivors than in the reference population over the entire follow-up period (3.34 vs 1.89).
- Over the entire study period, dementia was 76% more likely among stroke patients (hazard ratio [HR], 1.76; 95% CI, 1.73-1.79) and 82% more likely in the AMI cohort (HR, 1.82; 95% CI, 1.79-1.85) than in the reference population.
- Time-varying analysis revealed that dementia risk was highest within the first year after stroke, with a > 2.5-fold increase at 6 months (HR, 2.51; 95% CI, 2.42-2.59), which decreased to a 1.5-fold increase at 5 years (HR, 1.51; 95% CI, 1.48-1.56) but remained elevated compared with the reference population even 20 years after the index stroke.
- Recurrent stroke was associated with an approximately threefold increased risk for dementia (single recurrent stroke adjusted HR, 2.64; 95% CI, 2.54-2.74; multiple recurrent strokes adjusted HR, 3.05; 95% CI, 2.81-3.33).
IN PRACTICE:
“While much research has been focused on reducing the risk of a second stroke, our findings make it clear that more research also is needed on developing interventions to help prevent dementia after stroke,” lead author Raed A. Joundi, MD, DPhil, McMaster University, Hamilton, Ontario, Canada, said in a press release.
“There is a need to accelerate the implementation of promising interventions or multipronged approaches into large randomized controlled trials to lower the risk of dementia,” the investigators wrote.
SOURCE:
The study was published online on December 4 in Neurology.
LIMITATIONS:
The study’s limitations included reliance on administrative coding without imaging data, potential underestimation of mild dementia, and lack of granular information on stroke severity, disability, and prestroke cognitive decline. While adjustments were made for healthcare contact and secondary prevention medications, residual biases may have persisted.
DISCLOSURES:
This study received funding from the Canada Brain Research Fund, Heart & Stroke Foundation of Canada, and Canadian Stroke Consortium. Two authors hold awards and positions from national organizations and academic institutions in Canada. Additional details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Risk for dementia is nearly 80% higher in stroke survivors than in those without stroke, a new study reveals. The data suggest risk declines within 1 year after stroke but remains elevated for up to 20 years.
METHODOLOGY:
- Researchers conducted a population-wide analysis of over 15 million people in Canada between 2002 and 2022. The study focused on adults hospitalized for ischemic stroke, intracerebral hemorrhage, or acute myocardial infarction (AMI).
- Of 175,980 stroke survivors, 99% were matched 1:1 to residents without stroke on the basis of age, sex, rural residence, neighborhood deprivation, and vascular comorbidities. In addition, 90% of patients were matched to those with AMI.
- Incident dementia diagnoses were tracked starting 90 days after stroke until death, emigration, or the end of the study, using a validated algorithm based on hospitalization for dementia, prescriptions for cholinesterase inhibitors, or physician claims within 2 years.
- The mean follow-up duration was 5.6 years.
TAKEAWAY:
- Among stroke survivors, 19% were diagnosed with dementia vs 12.5% in the reference population. The dementia rate per 100 person-years was higher among stroke survivors than in the reference population over the entire follow-up period (3.34 vs 1.89).
- Over the entire study period, dementia was 76% more likely among stroke patients (hazard ratio [HR], 1.76; 95% CI, 1.73-1.79) and 82% more likely in the AMI cohort (HR, 1.82; 95% CI, 1.79-1.85) than in the reference population.
- Time-varying analysis revealed that dementia risk was highest within the first year after stroke, with a > 2.5-fold increase at 6 months (HR, 2.51; 95% CI, 2.42-2.59), which decreased to a 1.5-fold increase at 5 years (HR, 1.51; 95% CI, 1.48-1.56) but remained elevated compared with the reference population even 20 years after the index stroke.
- Recurrent stroke was associated with an approximately threefold increased risk for dementia (single recurrent stroke adjusted HR, 2.64; 95% CI, 2.54-2.74; multiple recurrent strokes adjusted HR, 3.05; 95% CI, 2.81-3.33).
IN PRACTICE:
“While much research has been focused on reducing the risk of a second stroke, our findings make it clear that more research also is needed on developing interventions to help prevent dementia after stroke,” lead author Raed A. Joundi, MD, DPhil, McMaster University, Hamilton, Ontario, Canada, said in a press release.
“There is a need to accelerate the implementation of promising interventions or multipronged approaches into large randomized controlled trials to lower the risk of dementia,” the investigators wrote.
SOURCE:
The study was published online on December 4 in Neurology.
LIMITATIONS:
The study’s limitations included reliance on administrative coding without imaging data, potential underestimation of mild dementia, and lack of granular information on stroke severity, disability, and prestroke cognitive decline. While adjustments were made for healthcare contact and secondary prevention medications, residual biases may have persisted.
DISCLOSURES:
This study received funding from the Canada Brain Research Fund, Heart & Stroke Foundation of Canada, and Canadian Stroke Consortium. Two authors hold awards and positions from national organizations and academic institutions in Canada. Additional details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.