User login
Recurrent Instability Seen in Intercollegiate Athletes With Shoulder Injury After Return to Play
SEATTLE—Among mid-season contact athletes with shoulder instability, 73% of athletes return to play after 1 week, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Regardless of whether the initial injury was a subluxation or dislocation, 63% of the cases developed recurrent instability.
There is no consensus on the optimal treatment of young in-season athletes with anterior shoulder instability and limited data are available to guide return to play and treatment. MAJ Jonathan F. Dickens, MD, from the John A. Feagin Jr. Sports Medicine Fellowship and Keller Army Hospital in West Point, New York, and colleagues conducted a study to examine the likelihood of return to sport following an in-season shoulder instability event based on the type of instability (subluxation vs. dislocation). Additionally, injury factors and patient reported outcome scores administered at the time of injury were evaluated to assess the predictability of eventual successful return to sport and time to return to sport during the competitive season following injury.
Dr. Dickens and colleagues examined 45 male and female intercollegiate athletes over 2 academic years, to assess return to play following in-season anterior glenohumeral instability. Athletes included in the sample were both male and female and participated in sports including basketball, soccer, lacrosse, and football. All observed athletes underwent a standardized accelerated rehabilitation program without shoulder immobilization, following the initial shoulder instability event. Subjects were followed during the course of their competitive season to determine return to play success and recurrent instability.
Of the 45 athletes who suffered an anterior shoulder instability event, 33 (73%) returned to play for at least part of the season after a median 5 days lost from competition. “While a large portion of the athletes in this observational study return to mid-season sport, only 36% completed the season without subsequent instability,” said Dr. Dickens. Athletes with a subluxation injury (partial dislocation) of the shoulder were 5.3 times more likely to return in the same season compared to those with a complete dislocation. The most common reason for athletes not returning was the inability to reach sufficient shoulder function for athletic participation.
“These early results should be valuable to physicians caring for the in-season athlete with shoulder instability, as we have not yet reached a consensus treatment approach on these injuries,” said Dr. Dickens. “More research is needed to determine the effect of multiple recurrent instability events on long-term outcomes and this study will hopefully be a first good step in understanding this relationship.”
SEATTLE—Among mid-season contact athletes with shoulder instability, 73% of athletes return to play after 1 week, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Regardless of whether the initial injury was a subluxation or dislocation, 63% of the cases developed recurrent instability.
There is no consensus on the optimal treatment of young in-season athletes with anterior shoulder instability and limited data are available to guide return to play and treatment. MAJ Jonathan F. Dickens, MD, from the John A. Feagin Jr. Sports Medicine Fellowship and Keller Army Hospital in West Point, New York, and colleagues conducted a study to examine the likelihood of return to sport following an in-season shoulder instability event based on the type of instability (subluxation vs. dislocation). Additionally, injury factors and patient reported outcome scores administered at the time of injury were evaluated to assess the predictability of eventual successful return to sport and time to return to sport during the competitive season following injury.
Dr. Dickens and colleagues examined 45 male and female intercollegiate athletes over 2 academic years, to assess return to play following in-season anterior glenohumeral instability. Athletes included in the sample were both male and female and participated in sports including basketball, soccer, lacrosse, and football. All observed athletes underwent a standardized accelerated rehabilitation program without shoulder immobilization, following the initial shoulder instability event. Subjects were followed during the course of their competitive season to determine return to play success and recurrent instability.
Of the 45 athletes who suffered an anterior shoulder instability event, 33 (73%) returned to play for at least part of the season after a median 5 days lost from competition. “While a large portion of the athletes in this observational study return to mid-season sport, only 36% completed the season without subsequent instability,” said Dr. Dickens. Athletes with a subluxation injury (partial dislocation) of the shoulder were 5.3 times more likely to return in the same season compared to those with a complete dislocation. The most common reason for athletes not returning was the inability to reach sufficient shoulder function for athletic participation.
“These early results should be valuable to physicians caring for the in-season athlete with shoulder instability, as we have not yet reached a consensus treatment approach on these injuries,” said Dr. Dickens. “More research is needed to determine the effect of multiple recurrent instability events on long-term outcomes and this study will hopefully be a first good step in understanding this relationship.”
SEATTLE—Among mid-season contact athletes with shoulder instability, 73% of athletes return to play after 1 week, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Regardless of whether the initial injury was a subluxation or dislocation, 63% of the cases developed recurrent instability.
There is no consensus on the optimal treatment of young in-season athletes with anterior shoulder instability and limited data are available to guide return to play and treatment. MAJ Jonathan F. Dickens, MD, from the John A. Feagin Jr. Sports Medicine Fellowship and Keller Army Hospital in West Point, New York, and colleagues conducted a study to examine the likelihood of return to sport following an in-season shoulder instability event based on the type of instability (subluxation vs. dislocation). Additionally, injury factors and patient reported outcome scores administered at the time of injury were evaluated to assess the predictability of eventual successful return to sport and time to return to sport during the competitive season following injury.
Dr. Dickens and colleagues examined 45 male and female intercollegiate athletes over 2 academic years, to assess return to play following in-season anterior glenohumeral instability. Athletes included in the sample were both male and female and participated in sports including basketball, soccer, lacrosse, and football. All observed athletes underwent a standardized accelerated rehabilitation program without shoulder immobilization, following the initial shoulder instability event. Subjects were followed during the course of their competitive season to determine return to play success and recurrent instability.
Of the 45 athletes who suffered an anterior shoulder instability event, 33 (73%) returned to play for at least part of the season after a median 5 days lost from competition. “While a large portion of the athletes in this observational study return to mid-season sport, only 36% completed the season without subsequent instability,” said Dr. Dickens. Athletes with a subluxation injury (partial dislocation) of the shoulder were 5.3 times more likely to return in the same season compared to those with a complete dislocation. The most common reason for athletes not returning was the inability to reach sufficient shoulder function for athletic participation.
“These early results should be valuable to physicians caring for the in-season athlete with shoulder instability, as we have not yet reached a consensus treatment approach on these injuries,” said Dr. Dickens. “More research is needed to determine the effect of multiple recurrent instability events on long-term outcomes and this study will hopefully be a first good step in understanding this relationship.”
Return to Play Rates Are High for NFL Players Following Shoulder Stabilization Surgery
SEATTLE—The return to play rates for National Football League (NFL) athletes following shoulder stabilization is approximately 90%, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. There is no difference in return to play rates between open and arthroscopic repairs.
Shoulder instability is a common injury among football players but the rate of return to play has not been regularly determined following surgery. Matthew J. White, MD, from the American Sports Medicine Institute (ASMI) in Birmingham, AL, and colleagues conducted a study to highlight the success rate of return to play in the NFL following shoulder stabilization surgery, and to determine what factors may affect return to play in these professional athletes.
Sixty NFL players who had undergone shoulder stabilization at ASMI were followed to determine the rate of return to play and the factors predicting return to play. Researchers performed chart review and analyzed follow-up data by accessing the NFL statistics database. Successful return to play was defined as participation in at least 1 regular season NFL game following surgery. Chi square and t-tests were performed to examine differences between perioperative and athletic history variables and a player’s ability to return to play. “Age, number of games before surgery, and career length were not statistically different between those that returned and those that did not,” said Dr. White.
Ninety percent (54 of 60) of NFL players were able to return to play following shoulder stabilization, with an average return to play time of 8.6 months. Eleven of the 60 patients underwent open stabilization. Ninety-two percent (45/49) of the arthroscopically treated and 82% (9/11) of the openly treated athletes were able to return to play. “It was also interesting to note, that players selected before the fourth round of the NFL draft were 7.6 times more likely to return to play following shoulder stabilization surgery,” said Dr. White.
In addition, circumferential labral tears were found in 7 athletes, all of whom returned to play following surgery. “Additional investigation on shoulder function and outcome scores long-term would be beneficial in this group of athletes to determine better standards of care,” noted Dr. White.
SEATTLE—The return to play rates for National Football League (NFL) athletes following shoulder stabilization is approximately 90%, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. There is no difference in return to play rates between open and arthroscopic repairs.
Shoulder instability is a common injury among football players but the rate of return to play has not been regularly determined following surgery. Matthew J. White, MD, from the American Sports Medicine Institute (ASMI) in Birmingham, AL, and colleagues conducted a study to highlight the success rate of return to play in the NFL following shoulder stabilization surgery, and to determine what factors may affect return to play in these professional athletes.
Sixty NFL players who had undergone shoulder stabilization at ASMI were followed to determine the rate of return to play and the factors predicting return to play. Researchers performed chart review and analyzed follow-up data by accessing the NFL statistics database. Successful return to play was defined as participation in at least 1 regular season NFL game following surgery. Chi square and t-tests were performed to examine differences between perioperative and athletic history variables and a player’s ability to return to play. “Age, number of games before surgery, and career length were not statistically different between those that returned and those that did not,” said Dr. White.
Ninety percent (54 of 60) of NFL players were able to return to play following shoulder stabilization, with an average return to play time of 8.6 months. Eleven of the 60 patients underwent open stabilization. Ninety-two percent (45/49) of the arthroscopically treated and 82% (9/11) of the openly treated athletes were able to return to play. “It was also interesting to note, that players selected before the fourth round of the NFL draft were 7.6 times more likely to return to play following shoulder stabilization surgery,” said Dr. White.
In addition, circumferential labral tears were found in 7 athletes, all of whom returned to play following surgery. “Additional investigation on shoulder function and outcome scores long-term would be beneficial in this group of athletes to determine better standards of care,” noted Dr. White.
SEATTLE—The return to play rates for National Football League (NFL) athletes following shoulder stabilization is approximately 90%, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. There is no difference in return to play rates between open and arthroscopic repairs.
Shoulder instability is a common injury among football players but the rate of return to play has not been regularly determined following surgery. Matthew J. White, MD, from the American Sports Medicine Institute (ASMI) in Birmingham, AL, and colleagues conducted a study to highlight the success rate of return to play in the NFL following shoulder stabilization surgery, and to determine what factors may affect return to play in these professional athletes.
Sixty NFL players who had undergone shoulder stabilization at ASMI were followed to determine the rate of return to play and the factors predicting return to play. Researchers performed chart review and analyzed follow-up data by accessing the NFL statistics database. Successful return to play was defined as participation in at least 1 regular season NFL game following surgery. Chi square and t-tests were performed to examine differences between perioperative and athletic history variables and a player’s ability to return to play. “Age, number of games before surgery, and career length were not statistically different between those that returned and those that did not,” said Dr. White.
Ninety percent (54 of 60) of NFL players were able to return to play following shoulder stabilization, with an average return to play time of 8.6 months. Eleven of the 60 patients underwent open stabilization. Ninety-two percent (45/49) of the arthroscopically treated and 82% (9/11) of the openly treated athletes were able to return to play. “It was also interesting to note, that players selected before the fourth round of the NFL draft were 7.6 times more likely to return to play following shoulder stabilization surgery,” said Dr. White.
In addition, circumferential labral tears were found in 7 athletes, all of whom returned to play following surgery. “Additional investigation on shoulder function and outcome scores long-term would be beneficial in this group of athletes to determine better standards of care,” noted Dr. White.
Increased Risk of Elbow Surgery for MLB Pitchers
SEATTLE— Eighty-seven percent of Major League Baseball (MLB) pitchers who underwent ulnar collateral ligament (UCL) reconstructive surgery returned to the Major League level of sport, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. However, the study also documented a decline in pitching performance after undergoing reconstructive surgery. Entering the Major Leagues at a younger age also increased a player’s risk for requiring surgery.
A tremendous amount of stress is placed on the elbow while pitching a baseball. Due to these stresses, MLB pitchers are at increased risk for UCL injuries. Robert A. Keller, MD, of Henry Ford Hospital in Detroit, Michigan, and colleagues, reviewed the statistics for 168 MLB pitchers, who threw at least 1 season at the Major League level and underwent UCL reconstruction. Statistical data, including earned run average (ERA), walks and hits per innings pitched (WHIP), win percentage, innings pitched, and salary were compared for the 3 years before and 3 years after undergoing UCL reconstruction. “Having athletic trainers and team physicians closely look at when players pitching performance stats start to decrease may allow for steps to be taken with a pitcher before a surgery is needed,” said Dr. Keller.
Of the 87% of pitchers that returned to the Major League level after undergoing UCL reconstruction, a statistically significant decline in their ERA (P = 0.001), WHIP (P = 0.011), and innings pitched (P = 0.026) was seen compared to pre-reconstruction performance. Reconstructed pitchers also had a statistically decline in their pitching performance in the season before their surgery (ERA P = 0.014, WHIP P = 0.036, innings pitched P < 0.001, win percentage P = 0.004). Approximately 60% of pitchers requiring UCL reconstruction had surgery within the first 5 years of being in the Major Leagues. Validated by a multivariable generalized estimating equation model that examined risk factors, arm stress from earlier Major League experience contributed to injury. In addition, players who entered the MLB at an earlier age also appeared to have a greater risk for surgery.
“Our results suggest that UCL reconstructive surgery does a tremendous job in allowing players to return to their same level of sport but it also describes a decline in pitching performance after undergoing reconstruction,” said Dr. Keller. “Our study also further highlights the need for kids not to overuse their arms early in their pitching careers.”
SEATTLE— Eighty-seven percent of Major League Baseball (MLB) pitchers who underwent ulnar collateral ligament (UCL) reconstructive surgery returned to the Major League level of sport, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. However, the study also documented a decline in pitching performance after undergoing reconstructive surgery. Entering the Major Leagues at a younger age also increased a player’s risk for requiring surgery.
A tremendous amount of stress is placed on the elbow while pitching a baseball. Due to these stresses, MLB pitchers are at increased risk for UCL injuries. Robert A. Keller, MD, of Henry Ford Hospital in Detroit, Michigan, and colleagues, reviewed the statistics for 168 MLB pitchers, who threw at least 1 season at the Major League level and underwent UCL reconstruction. Statistical data, including earned run average (ERA), walks and hits per innings pitched (WHIP), win percentage, innings pitched, and salary were compared for the 3 years before and 3 years after undergoing UCL reconstruction. “Having athletic trainers and team physicians closely look at when players pitching performance stats start to decrease may allow for steps to be taken with a pitcher before a surgery is needed,” said Dr. Keller.
Of the 87% of pitchers that returned to the Major League level after undergoing UCL reconstruction, a statistically significant decline in their ERA (P = 0.001), WHIP (P = 0.011), and innings pitched (P = 0.026) was seen compared to pre-reconstruction performance. Reconstructed pitchers also had a statistically decline in their pitching performance in the season before their surgery (ERA P = 0.014, WHIP P = 0.036, innings pitched P < 0.001, win percentage P = 0.004). Approximately 60% of pitchers requiring UCL reconstruction had surgery within the first 5 years of being in the Major Leagues. Validated by a multivariable generalized estimating equation model that examined risk factors, arm stress from earlier Major League experience contributed to injury. In addition, players who entered the MLB at an earlier age also appeared to have a greater risk for surgery.
“Our results suggest that UCL reconstructive surgery does a tremendous job in allowing players to return to their same level of sport but it also describes a decline in pitching performance after undergoing reconstruction,” said Dr. Keller. “Our study also further highlights the need for kids not to overuse their arms early in their pitching careers.”
SEATTLE— Eighty-seven percent of Major League Baseball (MLB) pitchers who underwent ulnar collateral ligament (UCL) reconstructive surgery returned to the Major League level of sport, according to a study presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. However, the study also documented a decline in pitching performance after undergoing reconstructive surgery. Entering the Major Leagues at a younger age also increased a player’s risk for requiring surgery.
A tremendous amount of stress is placed on the elbow while pitching a baseball. Due to these stresses, MLB pitchers are at increased risk for UCL injuries. Robert A. Keller, MD, of Henry Ford Hospital in Detroit, Michigan, and colleagues, reviewed the statistics for 168 MLB pitchers, who threw at least 1 season at the Major League level and underwent UCL reconstruction. Statistical data, including earned run average (ERA), walks and hits per innings pitched (WHIP), win percentage, innings pitched, and salary were compared for the 3 years before and 3 years after undergoing UCL reconstruction. “Having athletic trainers and team physicians closely look at when players pitching performance stats start to decrease may allow for steps to be taken with a pitcher before a surgery is needed,” said Dr. Keller.
Of the 87% of pitchers that returned to the Major League level after undergoing UCL reconstruction, a statistically significant decline in their ERA (P = 0.001), WHIP (P = 0.011), and innings pitched (P = 0.026) was seen compared to pre-reconstruction performance. Reconstructed pitchers also had a statistically decline in their pitching performance in the season before their surgery (ERA P = 0.014, WHIP P = 0.036, innings pitched P < 0.001, win percentage P = 0.004). Approximately 60% of pitchers requiring UCL reconstruction had surgery within the first 5 years of being in the Major Leagues. Validated by a multivariable generalized estimating equation model that examined risk factors, arm stress from earlier Major League experience contributed to injury. In addition, players who entered the MLB at an earlier age also appeared to have a greater risk for surgery.
“Our results suggest that UCL reconstructive surgery does a tremendous job in allowing players to return to their same level of sport but it also describes a decline in pitching performance after undergoing reconstruction,” said Dr. Keller. “Our study also further highlights the need for kids not to overuse their arms early in their pitching careers.”
New Research Identifies Risk Factors and Treatment Options for Little League Shoulder
SEATTLE—Proximal humeral epiphysiolysis, or little league shoulder (LLS), is being diagnosed with increasing frequency, according to data presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Concomitant elbow pain may also be seen in up to 13% of youth athletes diagnosed with LLS. After rest and physical therapy, recurrent symptoms can occur, generally 6 to 12 months after return to sports.
With rising participation in youth sports such as baseball and tennis, there remains a paucity of literature regarding the causes or outcomes of LLS. Benton E. Heyworth, MD, from Children’s Hospital Boston, Division of Sports Medicine in Boston, Massachusetts, and colleagues examined 95 patients with LLS. The researchers reviewed cases of LLS between 1999 and 2013 at a single pediatric referral center. The study analyzed age, sex, physical examination, radiologic findings, treatment approaches, and rates of recurrence.
Of the 95 patients (93 males; mean age 13.1 years, range 8-17 years), 13% reported elbow pain, 10% reported shoulder fatigue or weakness, 8% reported mechanical symptoms, and all patients complained of shoulder pain with overhead athletics. “These related symptoms should be recognized as possible identifiers for injured athletes in the future,” said Dr. Heyworth. On physical examination, 30% were reported to have glenohumeral internal rotation deficit (GIRD). Patients with GIRD were 3 times more likely to experience an injury recurrence 6 to 12 months after returning to play. “Not surprisingly, we found 97% of the affected athletes were baseball players, with 50% of the patients being only 12 or 13 years old—a good indicator of the stress being put on young arms,” added Dr. Heyworth.
Treatment recommendations included rest in 98% of cases, physical therapy in 79%, and position change upon return to play in 25%. Average time to resolution of symptoms was 2.6 months, with average time for return to competition was 4.2 months. Recurrent symptoms were reported in 7.4% in the overall population at a mean of 8 months following symptom resolution.
SEATTLE—Proximal humeral epiphysiolysis, or little league shoulder (LLS), is being diagnosed with increasing frequency, according to data presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Concomitant elbow pain may also be seen in up to 13% of youth athletes diagnosed with LLS. After rest and physical therapy, recurrent symptoms can occur, generally 6 to 12 months after return to sports.
With rising participation in youth sports such as baseball and tennis, there remains a paucity of literature regarding the causes or outcomes of LLS. Benton E. Heyworth, MD, from Children’s Hospital Boston, Division of Sports Medicine in Boston, Massachusetts, and colleagues examined 95 patients with LLS. The researchers reviewed cases of LLS between 1999 and 2013 at a single pediatric referral center. The study analyzed age, sex, physical examination, radiologic findings, treatment approaches, and rates of recurrence.
Of the 95 patients (93 males; mean age 13.1 years, range 8-17 years), 13% reported elbow pain, 10% reported shoulder fatigue or weakness, 8% reported mechanical symptoms, and all patients complained of shoulder pain with overhead athletics. “These related symptoms should be recognized as possible identifiers for injured athletes in the future,” said Dr. Heyworth. On physical examination, 30% were reported to have glenohumeral internal rotation deficit (GIRD). Patients with GIRD were 3 times more likely to experience an injury recurrence 6 to 12 months after returning to play. “Not surprisingly, we found 97% of the affected athletes were baseball players, with 50% of the patients being only 12 or 13 years old—a good indicator of the stress being put on young arms,” added Dr. Heyworth.
Treatment recommendations included rest in 98% of cases, physical therapy in 79%, and position change upon return to play in 25%. Average time to resolution of symptoms was 2.6 months, with average time for return to competition was 4.2 months. Recurrent symptoms were reported in 7.4% in the overall population at a mean of 8 months following symptom resolution.
SEATTLE—Proximal humeral epiphysiolysis, or little league shoulder (LLS), is being diagnosed with increasing frequency, according to data presented at the 2014 Annual Meeting of the American Orthopaedic Society for Sports Medicine. Concomitant elbow pain may also be seen in up to 13% of youth athletes diagnosed with LLS. After rest and physical therapy, recurrent symptoms can occur, generally 6 to 12 months after return to sports.
With rising participation in youth sports such as baseball and tennis, there remains a paucity of literature regarding the causes or outcomes of LLS. Benton E. Heyworth, MD, from Children’s Hospital Boston, Division of Sports Medicine in Boston, Massachusetts, and colleagues examined 95 patients with LLS. The researchers reviewed cases of LLS between 1999 and 2013 at a single pediatric referral center. The study analyzed age, sex, physical examination, radiologic findings, treatment approaches, and rates of recurrence.
Of the 95 patients (93 males; mean age 13.1 years, range 8-17 years), 13% reported elbow pain, 10% reported shoulder fatigue or weakness, 8% reported mechanical symptoms, and all patients complained of shoulder pain with overhead athletics. “These related symptoms should be recognized as possible identifiers for injured athletes in the future,” said Dr. Heyworth. On physical examination, 30% were reported to have glenohumeral internal rotation deficit (GIRD). Patients with GIRD were 3 times more likely to experience an injury recurrence 6 to 12 months after returning to play. “Not surprisingly, we found 97% of the affected athletes were baseball players, with 50% of the patients being only 12 or 13 years old—a good indicator of the stress being put on young arms,” added Dr. Heyworth.
Treatment recommendations included rest in 98% of cases, physical therapy in 79%, and position change upon return to play in 25%. Average time to resolution of symptoms was 2.6 months, with average time for return to competition was 4.2 months. Recurrent symptoms were reported in 7.4% in the overall population at a mean of 8 months following symptom resolution.
Acetaminophen no better than placebo for acute low back pain
Acetaminophen taken regularly or as required was no better than placebo in improving time to recovery in patients with acute low back pain, Australian research shows.
A randomized, placebo-controlled, double-dummy study in 1,643 patients presenting with acute low back pain found the median time to recovery was 17 days, both in patients assigned to 665 mg acetaminophen three times daily and in those told to take acetaminophen as required, and was 16 days in the placebo group.
After 12 weeks, similar numbers of patients in each group had achieved sustained recovery: 84.7% of participants taking regular acetaminophen, 82.8% of patients taking acetaminophen as required, and 84.3% of the placebo group.
"The clinical implications of PACE [Paracetamol for Low-Back Pain Study] require careful consideration of the efficacy of paracetamol [acetaminophen] with respect to the safe use of medicines for low back pain," the study authors wrote in the Lancet (2014 July 24 [doi:10.1016/ S0140-6736(14)60805-9]).
Acetaminophen traditionally has been recommended over anti-inflammatory medication because the side effect profile is safer, noted study coauthor Chung-Wei Christine Lin, Ph.D. However, the recommendation for its use in low back pain has come from indirect evidence in other pain conditions.
"Our advice to patients should be that for back pain, the prognosis is mostly good, most people recover reasonably well, they should stay active, and they should avoid bed rest," said Dr. Lin of the George Institute for Global Health, University of Sydney. "Beyond that, the emphasis on taking pain relief should probably be reduced, because taking pain relief doesn’t really do much beyond placebo."
A previous Cochrane review examining the use of anti-inflammatories for short-term pain relief found only a small effect, Dr. Lin noted, and other direct comparisons between anti-inflammatories and acetaminophen have shown no differences in effects.
"Patients should weigh the benefits of taking medicine for a small amount pain relief against the potential side effects and discuss this with their doctor or pharmacist" she cautioned.
The National Health and Medical Research Council of Australia and GlaxoSmithKline funded the study. Dr. Lin had no relevant financial disclosures.
Acetaminophen taken regularly or as required was no better than placebo in improving time to recovery in patients with acute low back pain, Australian research shows.
A randomized, placebo-controlled, double-dummy study in 1,643 patients presenting with acute low back pain found the median time to recovery was 17 days, both in patients assigned to 665 mg acetaminophen three times daily and in those told to take acetaminophen as required, and was 16 days in the placebo group.
After 12 weeks, similar numbers of patients in each group had achieved sustained recovery: 84.7% of participants taking regular acetaminophen, 82.8% of patients taking acetaminophen as required, and 84.3% of the placebo group.
"The clinical implications of PACE [Paracetamol for Low-Back Pain Study] require careful consideration of the efficacy of paracetamol [acetaminophen] with respect to the safe use of medicines for low back pain," the study authors wrote in the Lancet (2014 July 24 [doi:10.1016/ S0140-6736(14)60805-9]).
Acetaminophen traditionally has been recommended over anti-inflammatory medication because the side effect profile is safer, noted study coauthor Chung-Wei Christine Lin, Ph.D. However, the recommendation for its use in low back pain has come from indirect evidence in other pain conditions.
"Our advice to patients should be that for back pain, the prognosis is mostly good, most people recover reasonably well, they should stay active, and they should avoid bed rest," said Dr. Lin of the George Institute for Global Health, University of Sydney. "Beyond that, the emphasis on taking pain relief should probably be reduced, because taking pain relief doesn’t really do much beyond placebo."
A previous Cochrane review examining the use of anti-inflammatories for short-term pain relief found only a small effect, Dr. Lin noted, and other direct comparisons between anti-inflammatories and acetaminophen have shown no differences in effects.
"Patients should weigh the benefits of taking medicine for a small amount pain relief against the potential side effects and discuss this with their doctor or pharmacist" she cautioned.
The National Health and Medical Research Council of Australia and GlaxoSmithKline funded the study. Dr. Lin had no relevant financial disclosures.
Acetaminophen taken regularly or as required was no better than placebo in improving time to recovery in patients with acute low back pain, Australian research shows.
A randomized, placebo-controlled, double-dummy study in 1,643 patients presenting with acute low back pain found the median time to recovery was 17 days, both in patients assigned to 665 mg acetaminophen three times daily and in those told to take acetaminophen as required, and was 16 days in the placebo group.
After 12 weeks, similar numbers of patients in each group had achieved sustained recovery: 84.7% of participants taking regular acetaminophen, 82.8% of patients taking acetaminophen as required, and 84.3% of the placebo group.
"The clinical implications of PACE [Paracetamol for Low-Back Pain Study] require careful consideration of the efficacy of paracetamol [acetaminophen] with respect to the safe use of medicines for low back pain," the study authors wrote in the Lancet (2014 July 24 [doi:10.1016/ S0140-6736(14)60805-9]).
Acetaminophen traditionally has been recommended over anti-inflammatory medication because the side effect profile is safer, noted study coauthor Chung-Wei Christine Lin, Ph.D. However, the recommendation for its use in low back pain has come from indirect evidence in other pain conditions.
"Our advice to patients should be that for back pain, the prognosis is mostly good, most people recover reasonably well, they should stay active, and they should avoid bed rest," said Dr. Lin of the George Institute for Global Health, University of Sydney. "Beyond that, the emphasis on taking pain relief should probably be reduced, because taking pain relief doesn’t really do much beyond placebo."
A previous Cochrane review examining the use of anti-inflammatories for short-term pain relief found only a small effect, Dr. Lin noted, and other direct comparisons between anti-inflammatories and acetaminophen have shown no differences in effects.
"Patients should weigh the benefits of taking medicine for a small amount pain relief against the potential side effects and discuss this with their doctor or pharmacist" she cautioned.
The National Health and Medical Research Council of Australia and GlaxoSmithKline funded the study. Dr. Lin had no relevant financial disclosures.
FROM THE LANCET
Key clinical point: Acetaminophen may offer no pain-relief advantage in acute low back pain.
Major finding: 84.8% of patients with acute low back pain who took regular acetaminophen, 82.7% of patients taking acetaminophen as required, and 84.2% taking placebo achieved sustained recovery after 12 weeks.
Data source: Randomized, placebo-controlled, double-blind, double-dummy study of 1,643 patients with acute low back pain.
Disclosures: The National Health and Medical Research Council of Australia and GlaxoSmithKline funded the study. Dr. Lin had no relevant financial disclosures.
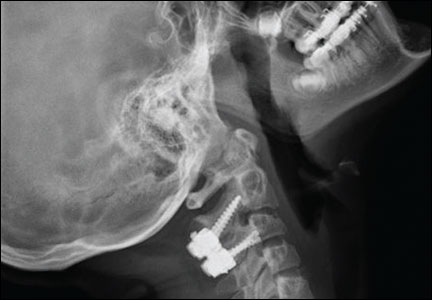
Spontaneous Septic Arthritis of the Lumbar Facet Caused by Methicillin-Resistant Staphylococcus aureus in an Otherwise Healthy Adolescent
Editorial: A Night (and Week) to Remember!
Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?

Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?

Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?