User login
Geographic Clusters Show Uneven Cancer Screening in the US
Geographic Clusters Show Uneven Cancer Screening in the US
TOPLINE:
An analysis of 3142 US counties revealed that county-level screening for breast, cervical, and colorectal cancer increased overall between 1997 and 2019; however, despite the reduced geographic variation, persistently high-screening clusters remained in the Northeast, whereas persistently low-screening clusters remained in the Southwest.
METHODOLOGY:
- Cancer screening reduces mortality. Despite guideline recommendation, the uptake of breast, cervical, and colorectal cancer screening in the US falls short of national goals and varies across sociodemographic groups. To date, only a few studies have examined geographic and temporal patterns of screening.
- To address this gap, researchers conducted a cross-sectional study using an ecological panel design to analyze county-level screening prevalence across 3142 US mainland counties from 1997 to 2019, deriving prevalence estimates from Behavioral Risk Factor Surveillance System (BRFSS) and National Health Interview Survey (NHIS) data over 3- to 5-year periods.
- Spatial autocorrelation analyses, including Global Moran I and the bivariate local indicator of spatial autocorrelation, were performed to assess geographic clusters of cancer screening within each period. Four types of local geographic clusters of county-level cancer screening were identified: counties with persistently high screening rates, counties with persistently low screening rates, counties in which screening rates decreased from high to low, and counties in which screening rates increased from low to high.
- Screening prevalence was compared across multiple time windows for different modalities (mammography, a Papanicolaou test, colonoscopy, colorectal cancer test, endoscopy, and a fecal occult blood test [FOBT]). Overall, 3101 counties were analyzed for mammography and the Papanicolaou test, 3107 counties for colonoscopy, 3100 counties for colorectal cancer test, 3089 counties for endoscopy, and 3090 counties for the FOBT.
TAKEAWAY:
- Overall screening prevalence increased from 1997 to 2019, and global spatial autocorrelation declined over time. For instance, the distribution of mammography screening became 83% more uniform in more recent years (Moran I, 0.57 in 1997-1999 vs 0.10 in 2017-2019). Similarly, Papanicolaou test screening became more uniform in more recent years (Moran I, 0.44 vs. 0.07). These changes indicate reduced geographic heterogeneity.
- Colonoscopy and endoscopy use increased, surpassing a 50% prevalence in many counties for 2010; however, FOBT use declined. Spatial clustering also attenuated, with a 23.4% declined in Moran I for colonoscopy from 2011-2016 to 2017-2019, a 12.3% decline in the colorectal cancer test from 2004-2007 to 2008-2010, and a 14.0% decline for endoscopy from 2004-2007 to 2008-2010.
- Persistently high-/high-screening clusters were concentrated in the Northeast for mammography and colorectal cancer screening and in the East for Papanicolaou test screening, whereas persistently low-/low-screening clusters were concentrated in the Southwest for the same modalities.
- Clusters of low- and high-screening counties were more disadvantaged -- with lower socioeconomic status and a higher proportion of non-White residents -- than other cluster types, suggesting some improvement in screening uptake in more disadvantaged areas. Counties with persistently low screening exhibited greater socioeconomic disadvantages -- lower media household income, higher poverty, lower home values, and lower educational attainment -- than those with persistently high screening.
IN PRACTICE:
"This cross-sectional study found that despite secular increases that reduced geographic variation in screening, local clusters of high and low screening persisted in the Northeast and Southwest US, respectively. Future studies could incorporate health care access characteristics to explain why areas of low screening did not catch up to optimize cancer screening practice," the authors wrote.
SOURCE:
The study, led by Pranoti Pradhan, PhD, Harvard T.H. Chan School of Public Health, Boston, was published online in JAMA Network Open.
LIMITATIONS:
The county-level estimates were modeled using BRFSS, NHIS, and US Census data, which might be susceptible to sampling biases despite corrections for nonresponse and noncoverage. Researchers lacked data on specific health systems characteristics that may have directly driven changes in prevalence and were restricted to using screening time intervals available from the Small Area Estimates for Cancer-Relates Measures from the National Cancer Institute, rather than those according to US Preventive Services Task Force guidelines. Additionally, the spatial cluster method was sensitive to county size and arrangement, which may have influenced local cluster detection.
DISCLOSURES:
This research was supported by the T32 Cancer Prevention and Control Funding Fellowship and T32 Cancer Epidemiology Fellowship at the Harvard T.H. Chan School of Public Health. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
An analysis of 3142 US counties revealed that county-level screening for breast, cervical, and colorectal cancer increased overall between 1997 and 2019; however, despite the reduced geographic variation, persistently high-screening clusters remained in the Northeast, whereas persistently low-screening clusters remained in the Southwest.
METHODOLOGY:
- Cancer screening reduces mortality. Despite guideline recommendation, the uptake of breast, cervical, and colorectal cancer screening in the US falls short of national goals and varies across sociodemographic groups. To date, only a few studies have examined geographic and temporal patterns of screening.
- To address this gap, researchers conducted a cross-sectional study using an ecological panel design to analyze county-level screening prevalence across 3142 US mainland counties from 1997 to 2019, deriving prevalence estimates from Behavioral Risk Factor Surveillance System (BRFSS) and National Health Interview Survey (NHIS) data over 3- to 5-year periods.
- Spatial autocorrelation analyses, including Global Moran I and the bivariate local indicator of spatial autocorrelation, were performed to assess geographic clusters of cancer screening within each period. Four types of local geographic clusters of county-level cancer screening were identified: counties with persistently high screening rates, counties with persistently low screening rates, counties in which screening rates decreased from high to low, and counties in which screening rates increased from low to high.
- Screening prevalence was compared across multiple time windows for different modalities (mammography, a Papanicolaou test, colonoscopy, colorectal cancer test, endoscopy, and a fecal occult blood test [FOBT]). Overall, 3101 counties were analyzed for mammography and the Papanicolaou test, 3107 counties for colonoscopy, 3100 counties for colorectal cancer test, 3089 counties for endoscopy, and 3090 counties for the FOBT.
TAKEAWAY:
- Overall screening prevalence increased from 1997 to 2019, and global spatial autocorrelation declined over time. For instance, the distribution of mammography screening became 83% more uniform in more recent years (Moran I, 0.57 in 1997-1999 vs 0.10 in 2017-2019). Similarly, Papanicolaou test screening became more uniform in more recent years (Moran I, 0.44 vs. 0.07). These changes indicate reduced geographic heterogeneity.
- Colonoscopy and endoscopy use increased, surpassing a 50% prevalence in many counties for 2010; however, FOBT use declined. Spatial clustering also attenuated, with a 23.4% declined in Moran I for colonoscopy from 2011-2016 to 2017-2019, a 12.3% decline in the colorectal cancer test from 2004-2007 to 2008-2010, and a 14.0% decline for endoscopy from 2004-2007 to 2008-2010.
- Persistently high-/high-screening clusters were concentrated in the Northeast for mammography and colorectal cancer screening and in the East for Papanicolaou test screening, whereas persistently low-/low-screening clusters were concentrated in the Southwest for the same modalities.
- Clusters of low- and high-screening counties were more disadvantaged -- with lower socioeconomic status and a higher proportion of non-White residents -- than other cluster types, suggesting some improvement in screening uptake in more disadvantaged areas. Counties with persistently low screening exhibited greater socioeconomic disadvantages -- lower media household income, higher poverty, lower home values, and lower educational attainment -- than those with persistently high screening.
IN PRACTICE:
"This cross-sectional study found that despite secular increases that reduced geographic variation in screening, local clusters of high and low screening persisted in the Northeast and Southwest US, respectively. Future studies could incorporate health care access characteristics to explain why areas of low screening did not catch up to optimize cancer screening practice," the authors wrote.
SOURCE:
The study, led by Pranoti Pradhan, PhD, Harvard T.H. Chan School of Public Health, Boston, was published online in JAMA Network Open.
LIMITATIONS:
The county-level estimates were modeled using BRFSS, NHIS, and US Census data, which might be susceptible to sampling biases despite corrections for nonresponse and noncoverage. Researchers lacked data on specific health systems characteristics that may have directly driven changes in prevalence and were restricted to using screening time intervals available from the Small Area Estimates for Cancer-Relates Measures from the National Cancer Institute, rather than those according to US Preventive Services Task Force guidelines. Additionally, the spatial cluster method was sensitive to county size and arrangement, which may have influenced local cluster detection.
DISCLOSURES:
This research was supported by the T32 Cancer Prevention and Control Funding Fellowship and T32 Cancer Epidemiology Fellowship at the Harvard T.H. Chan School of Public Health. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
An analysis of 3142 US counties revealed that county-level screening for breast, cervical, and colorectal cancer increased overall between 1997 and 2019; however, despite the reduced geographic variation, persistently high-screening clusters remained in the Northeast, whereas persistently low-screening clusters remained in the Southwest.
METHODOLOGY:
- Cancer screening reduces mortality. Despite guideline recommendation, the uptake of breast, cervical, and colorectal cancer screening in the US falls short of national goals and varies across sociodemographic groups. To date, only a few studies have examined geographic and temporal patterns of screening.
- To address this gap, researchers conducted a cross-sectional study using an ecological panel design to analyze county-level screening prevalence across 3142 US mainland counties from 1997 to 2019, deriving prevalence estimates from Behavioral Risk Factor Surveillance System (BRFSS) and National Health Interview Survey (NHIS) data over 3- to 5-year periods.
- Spatial autocorrelation analyses, including Global Moran I and the bivariate local indicator of spatial autocorrelation, were performed to assess geographic clusters of cancer screening within each period. Four types of local geographic clusters of county-level cancer screening were identified: counties with persistently high screening rates, counties with persistently low screening rates, counties in which screening rates decreased from high to low, and counties in which screening rates increased from low to high.
- Screening prevalence was compared across multiple time windows for different modalities (mammography, a Papanicolaou test, colonoscopy, colorectal cancer test, endoscopy, and a fecal occult blood test [FOBT]). Overall, 3101 counties were analyzed for mammography and the Papanicolaou test, 3107 counties for colonoscopy, 3100 counties for colorectal cancer test, 3089 counties for endoscopy, and 3090 counties for the FOBT.
TAKEAWAY:
- Overall screening prevalence increased from 1997 to 2019, and global spatial autocorrelation declined over time. For instance, the distribution of mammography screening became 83% more uniform in more recent years (Moran I, 0.57 in 1997-1999 vs 0.10 in 2017-2019). Similarly, Papanicolaou test screening became more uniform in more recent years (Moran I, 0.44 vs. 0.07). These changes indicate reduced geographic heterogeneity.
- Colonoscopy and endoscopy use increased, surpassing a 50% prevalence in many counties for 2010; however, FOBT use declined. Spatial clustering also attenuated, with a 23.4% declined in Moran I for colonoscopy from 2011-2016 to 2017-2019, a 12.3% decline in the colorectal cancer test from 2004-2007 to 2008-2010, and a 14.0% decline for endoscopy from 2004-2007 to 2008-2010.
- Persistently high-/high-screening clusters were concentrated in the Northeast for mammography and colorectal cancer screening and in the East for Papanicolaou test screening, whereas persistently low-/low-screening clusters were concentrated in the Southwest for the same modalities.
- Clusters of low- and high-screening counties were more disadvantaged -- with lower socioeconomic status and a higher proportion of non-White residents -- than other cluster types, suggesting some improvement in screening uptake in more disadvantaged areas. Counties with persistently low screening exhibited greater socioeconomic disadvantages -- lower media household income, higher poverty, lower home values, and lower educational attainment -- than those with persistently high screening.
IN PRACTICE:
"This cross-sectional study found that despite secular increases that reduced geographic variation in screening, local clusters of high and low screening persisted in the Northeast and Southwest US, respectively. Future studies could incorporate health care access characteristics to explain why areas of low screening did not catch up to optimize cancer screening practice," the authors wrote.
SOURCE:
The study, led by Pranoti Pradhan, PhD, Harvard T.H. Chan School of Public Health, Boston, was published online in JAMA Network Open.
LIMITATIONS:
The county-level estimates were modeled using BRFSS, NHIS, and US Census data, which might be susceptible to sampling biases despite corrections for nonresponse and noncoverage. Researchers lacked data on specific health systems characteristics that may have directly driven changes in prevalence and were restricted to using screening time intervals available from the Small Area Estimates for Cancer-Relates Measures from the National Cancer Institute, rather than those according to US Preventive Services Task Force guidelines. Additionally, the spatial cluster method was sensitive to county size and arrangement, which may have influenced local cluster detection.
DISCLOSURES:
This research was supported by the T32 Cancer Prevention and Control Funding Fellowship and T32 Cancer Epidemiology Fellowship at the Harvard T.H. Chan School of Public Health. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
Geographic Clusters Show Uneven Cancer Screening in the US
Geographic Clusters Show Uneven Cancer Screening in the US
Improving Colorectal Cancer Screening via Mailed Fecal Immunochemical Testing in a Veterans Affairs Health System
Colorectal cancer (CRC) is among the most common cancers and causes of cancer-related deaths in the United States.1 Reflective of a nationwide trend, CRC screening rates at the Veterans Affairs Connecticut Healthcare System (VACHS) decreased during the COVID-19 pandemic.2-5 Contributing factors to this decrease included cancellations of elective colonoscopies during the initial phase of the pandemic and concurrent turnover of endoscopists. In 2021, the US Preventive Services Task Force lowered the recommended initial CRC screening age from 50 years to 45 years, further increasing the backlog of unscreened patients.6
Fecal immunochemical testing (FIT) is a noninvasive screening method in which antibodies are used to detect hemoglobin in the stool. The sensitivity and specificity of 1-time FIT are 79% to 80% and 94%, respectively, for the detection of CRC, with sensitivity improving with successive testing.7,8 Annual FIT is recognized as a tier 1 preferred screening method by the US Multi-Society Task Force on Colorectal Cancer.7,9 Programs that mail FIT kits to eligible patients outside of physician visits have been successfully implemented in health care systems.10,11
The VACHS designed and implemented a mailed FIT program using existing infrastructure and staffing.
Program Description
A team of local stakeholders comprised of VACHS leadership, primary care, nursing, and gastroenterology staff, as well as representatives from laboratory, informatics, mail services, and group practice management, was established to execute the project. The team met monthly to plan the project.
The team developed a dataset consisting of patients aged 45 to 75 years who were at average risk for CRC and due for CRC screening. Patients were defined as due for CRC screening if they had not had a colonoscopy in the previous 9 years or a FIT or fecal occult blood test in the previous 11 months. Average risk for CRC was defined by excluding patients with associated diagnosis codes for CRC, colectomy, inflammatory bowel disease, and anemia. The program also excluded patients with diagnosis codes associated with dementia, deferring discussions about cancer screening to their primary care practitioners (PCPs). Patients with invalid mailing addresses were also excluded, as well as those whose PCPs had indicated in the electronic health record that the patient received CRC screening outside the US Department of Veterans Affairs (VA) system.
Letter Templates
Two patient letter electronic health record templates were developed. The first was a primer letter, which was mailed to patients 2 to 3 weeks before the mailed FIT kit as an introduction to the program.12 The purpose of the primer letter was to give advance notice to patients that they could expect a FIT kit to arrive in the mail. The goal was to prepare patients to complete FIT when the kit arrived and prompt them to call the VA to opt out of the mailed FIT program if they were up to date with CRC screening or if they had a condition which made them at high risk for CRC.
The second FIT letter arrived with the FIT kit, introduced FIT and described the importance of CRC screening. The letter detailed instructions for completing FIT and automatically created a FIT order. It also included a list of common conditions that may exclude patients, with a recommendation for patients to contact their medical team if they felt they were not candidates for FIT.
Staff Education
A previous VACHS pilot project demonstrated the success of a mailed FIT program to increase FIT use. Implemented as part of the pilot program, staff education consisted of a session for clinicians about the role of FIT in CRC screening and an all-staff education session. An additional education session about CRC and FIT for all staff was repeated with the program launch.
Program Launch
The mailed FIT program was introduced during a VACHS primary care all-staff meeting. After the meeting, each patient aligned care team (PACT) received an encrypted email that included a list of the patients on their team who were candidates for the program, a patient-facing FIT instruction sheet, detailed instructions on how to send the FIT primer letter, and a FIT package consisting of the labeled FIT kit, FIT letter, and patient instruction sheet. A reminder letter was sent to each patient 3 weeks after the FIT package was mailed. The patient lists were populated into a shared, encrypted Microsoft Teams folder that was edited in real time by PACT teams and viewed by VACHS leadership to track progress.
Program Metrics
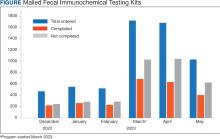
At program launch, the VACHS had 4642 patients due for CRC screening who were eligible for the mailed FIT program. On March 7, 2023, the data consisting of FIT tests ordered between December 2022 and May 2023—3 months before and after the launch of the program—were reviewed and categorized. In the 3 months before program launch, 1528 FIT were ordered and 714 were returned (46.7%). In the 3 months after the launch of the program, 4383 FIT were ordered and 1712 were returned (39.1%) (Figure). Test orders increased 287% from the preintervention to the postintervention period. The mean (SD) number of monthly FIT tests prelaunch was 509 (32.7), which increased to 1461 (331.6) postlaunch.
At the VACHS, 61.4% of patients aged 45 to 75 years were up to date with CRC screening before the program launch. In the 3 months after program launch, the rate increased to 63.8% among patients aged 45 to 75 years, the highest rate in our Veterans Integrated Services Network and exceeding the VA national average CRC screening rate, according to unpublished VA Monthly Management Report data.
In the 3 months following the program launch, 139 FIT kits tested positive for potential CRC. Of these, 79 (56.8%) patients had completed a diagnostic colonoscopy. PACT PCPs and nurses received reports on patients with positive FIT tests and those with no colonoscopy scheduled or completed and were asked to follow up.
Discussion
Through a proactive, population-based CRC screening program centered on mailed FIT kits outside of the traditional patient visit, the VACHS increased the use of FIT and rates of CRC screening. The numbers of FIT kits ordered and completed substantially increased in the 3 months after program launch.
Compared to mailed FIT programs described in the literature that rely on centralized processes in that a separate team operates the mailed FIT program for the entire organization, this program used existing PACT infrastructure and staff.10,11 This strategy allowed VACHS to design and implement the program in several months. Not needing to hire new staff or create a central team for the sole purpose of implementing the program allowed us to save on any organizational funding and efforts that would have accompanied the additional staff. The program described in this article may be more attainable for primary care practices or smaller health systems that do not have the capacity for the creation of a centralized process.
Limitations
Although the total number of FIT completions substantially increased during the program, the rate of FIT completion during the mailed FIT program was lower than the rate of completion prior to program launch. This decreased rate of FIT kit completion may be related to separation from a patient visit and potential loss of real-time education with a clinician. The program’s decentralized design increased the existing workload for primary care staff, and as a result, consideration must be given to local staffing levels. Additionally, the report of eligible patients depended on diagnosis codes and may have captured patients with higher-than-average risk of CRC, such as patients with prior history of adenomatous polyps, family history of CRC, or other medical or genetic conditions. We attempted to mitigate this by including a list of conditions that would exclude patients from FIT eligibility in the FIT letter and giving them the option to opt out.
Conclusions
CRC screening rates improved following implementation of a primary care team-centered quality improvement process to proactively identify patients appropriate for FIT and mail them FIT kits. This project highlights that population-health interventions around CRC screening via use of FIT can be successful within a primary care patient-centered medical home model, considering the increases in both CRC screening rates and increase in FIT tests ordered.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 29, 2024. Accessed June 11, 2024. https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html
2. Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-884. doi:10.1001/jamaoncol.2021.0884
3. Mazidimoradi A, Tiznobaik A, Salehiniya H. Impact of the COVID-19 pandemic on colorectal cancer screening: a systematic review. J Gastrointest Cancer. 2022;53(3):730-744. doi:10.1007/s12029-021-00679-x
4. Adams MA, Kurlander JE, Gao Y, Yankey N, Saini SD. Impact of coronavirus disease 2019 on screening colonoscopy utilization in a large integrated health system. Gastroenterology. 2022;162(7):2098-2100.e2. doi:10.1053/j.gastro.2022.02.034
5. Sundaram S, Olson S, Sharma P, Rajendra S. A review of the impact of the COVID-19 pandemic on colorectal cancer screening: implications and solutions. Pathogens. 2021;10(11):558. doi:10.3390/pathogens10111508
6. US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977. doi:10.1001/jama.2021.6238
7. Robertson DJ, Lee JK, Boland CR, et al. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2017;85(1):2-21.e3. doi:10.1016/j.gie.2016.09.025
8. Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160(3):171. doi:10.7326/M13-1484
9. Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153(1):307-323. doi:10.1053/j.gastro.2017.05.013
10. Deeds SA, Moore CB, Gunnink EJ, et al. Implementation of a mailed faecal immunochemical test programme for colorectal cancer screening among veterans. BMJ Open Qual. 2022;11(4):e001927. doi:10.1136/bmjoq-2022-001927
11. Selby K, Jensen CD, Levin TR, et al. Program components and results from an organized colorectal cancer screening program using annual fecal immunochemical testing. Clin Gastroenterol Hepatol. 2022;20(1):145-152. doi:10.1016/j.cgh.2020.09.042
12. Deeds S, Liu T, Schuttner L, et al. A postcard primer prior to mailed fecal immunochemical test among veterans: a randomized controlled trial. J Gen Intern Med. 2023:38(14):3235-3241. doi:10.1007/s11606-023-08248-7
Colorectal cancer (CRC) is among the most common cancers and causes of cancer-related deaths in the United States.1 Reflective of a nationwide trend, CRC screening rates at the Veterans Affairs Connecticut Healthcare System (VACHS) decreased during the COVID-19 pandemic.2-5 Contributing factors to this decrease included cancellations of elective colonoscopies during the initial phase of the pandemic and concurrent turnover of endoscopists. In 2021, the US Preventive Services Task Force lowered the recommended initial CRC screening age from 50 years to 45 years, further increasing the backlog of unscreened patients.6
Fecal immunochemical testing (FIT) is a noninvasive screening method in which antibodies are used to detect hemoglobin in the stool. The sensitivity and specificity of 1-time FIT are 79% to 80% and 94%, respectively, for the detection of CRC, with sensitivity improving with successive testing.7,8 Annual FIT is recognized as a tier 1 preferred screening method by the US Multi-Society Task Force on Colorectal Cancer.7,9 Programs that mail FIT kits to eligible patients outside of physician visits have been successfully implemented in health care systems.10,11
The VACHS designed and implemented a mailed FIT program using existing infrastructure and staffing.
Program Description
A team of local stakeholders comprised of VACHS leadership, primary care, nursing, and gastroenterology staff, as well as representatives from laboratory, informatics, mail services, and group practice management, was established to execute the project. The team met monthly to plan the project.
The team developed a dataset consisting of patients aged 45 to 75 years who were at average risk for CRC and due for CRC screening. Patients were defined as due for CRC screening if they had not had a colonoscopy in the previous 9 years or a FIT or fecal occult blood test in the previous 11 months. Average risk for CRC was defined by excluding patients with associated diagnosis codes for CRC, colectomy, inflammatory bowel disease, and anemia. The program also excluded patients with diagnosis codes associated with dementia, deferring discussions about cancer screening to their primary care practitioners (PCPs). Patients with invalid mailing addresses were also excluded, as well as those whose PCPs had indicated in the electronic health record that the patient received CRC screening outside the US Department of Veterans Affairs (VA) system.
Letter Templates
Two patient letter electronic health record templates were developed. The first was a primer letter, which was mailed to patients 2 to 3 weeks before the mailed FIT kit as an introduction to the program.12 The purpose of the primer letter was to give advance notice to patients that they could expect a FIT kit to arrive in the mail. The goal was to prepare patients to complete FIT when the kit arrived and prompt them to call the VA to opt out of the mailed FIT program if they were up to date with CRC screening or if they had a condition which made them at high risk for CRC.
The second FIT letter arrived with the FIT kit, introduced FIT and described the importance of CRC screening. The letter detailed instructions for completing FIT and automatically created a FIT order. It also included a list of common conditions that may exclude patients, with a recommendation for patients to contact their medical team if they felt they were not candidates for FIT.
Staff Education
A previous VACHS pilot project demonstrated the success of a mailed FIT program to increase FIT use. Implemented as part of the pilot program, staff education consisted of a session for clinicians about the role of FIT in CRC screening and an all-staff education session. An additional education session about CRC and FIT for all staff was repeated with the program launch.
Program Launch
The mailed FIT program was introduced during a VACHS primary care all-staff meeting. After the meeting, each patient aligned care team (PACT) received an encrypted email that included a list of the patients on their team who were candidates for the program, a patient-facing FIT instruction sheet, detailed instructions on how to send the FIT primer letter, and a FIT package consisting of the labeled FIT kit, FIT letter, and patient instruction sheet. A reminder letter was sent to each patient 3 weeks after the FIT package was mailed. The patient lists were populated into a shared, encrypted Microsoft Teams folder that was edited in real time by PACT teams and viewed by VACHS leadership to track progress.
Program Metrics
At program launch, the VACHS had 4642 patients due for CRC screening who were eligible for the mailed FIT program. On March 7, 2023, the data consisting of FIT tests ordered between December 2022 and May 2023—3 months before and after the launch of the program—were reviewed and categorized. In the 3 months before program launch, 1528 FIT were ordered and 714 were returned (46.7%). In the 3 months after the launch of the program, 4383 FIT were ordered and 1712 were returned (39.1%) (Figure). Test orders increased 287% from the preintervention to the postintervention period. The mean (SD) number of monthly FIT tests prelaunch was 509 (32.7), which increased to 1461 (331.6) postlaunch.
At the VACHS, 61.4% of patients aged 45 to 75 years were up to date with CRC screening before the program launch. In the 3 months after program launch, the rate increased to 63.8% among patients aged 45 to 75 years, the highest rate in our Veterans Integrated Services Network and exceeding the VA national average CRC screening rate, according to unpublished VA Monthly Management Report data.
In the 3 months following the program launch, 139 FIT kits tested positive for potential CRC. Of these, 79 (56.8%) patients had completed a diagnostic colonoscopy. PACT PCPs and nurses received reports on patients with positive FIT tests and those with no colonoscopy scheduled or completed and were asked to follow up.
Discussion
Through a proactive, population-based CRC screening program centered on mailed FIT kits outside of the traditional patient visit, the VACHS increased the use of FIT and rates of CRC screening. The numbers of FIT kits ordered and completed substantially increased in the 3 months after program launch.
Compared to mailed FIT programs described in the literature that rely on centralized processes in that a separate team operates the mailed FIT program for the entire organization, this program used existing PACT infrastructure and staff.10,11 This strategy allowed VACHS to design and implement the program in several months. Not needing to hire new staff or create a central team for the sole purpose of implementing the program allowed us to save on any organizational funding and efforts that would have accompanied the additional staff. The program described in this article may be more attainable for primary care practices or smaller health systems that do not have the capacity for the creation of a centralized process.
Limitations
Although the total number of FIT completions substantially increased during the program, the rate of FIT completion during the mailed FIT program was lower than the rate of completion prior to program launch. This decreased rate of FIT kit completion may be related to separation from a patient visit and potential loss of real-time education with a clinician. The program’s decentralized design increased the existing workload for primary care staff, and as a result, consideration must be given to local staffing levels. Additionally, the report of eligible patients depended on diagnosis codes and may have captured patients with higher-than-average risk of CRC, such as patients with prior history of adenomatous polyps, family history of CRC, or other medical or genetic conditions. We attempted to mitigate this by including a list of conditions that would exclude patients from FIT eligibility in the FIT letter and giving them the option to opt out.
Conclusions
CRC screening rates improved following implementation of a primary care team-centered quality improvement process to proactively identify patients appropriate for FIT and mail them FIT kits. This project highlights that population-health interventions around CRC screening via use of FIT can be successful within a primary care patient-centered medical home model, considering the increases in both CRC screening rates and increase in FIT tests ordered.
Colorectal cancer (CRC) is among the most common cancers and causes of cancer-related deaths in the United States.1 Reflective of a nationwide trend, CRC screening rates at the Veterans Affairs Connecticut Healthcare System (VACHS) decreased during the COVID-19 pandemic.2-5 Contributing factors to this decrease included cancellations of elective colonoscopies during the initial phase of the pandemic and concurrent turnover of endoscopists. In 2021, the US Preventive Services Task Force lowered the recommended initial CRC screening age from 50 years to 45 years, further increasing the backlog of unscreened patients.6
Fecal immunochemical testing (FIT) is a noninvasive screening method in which antibodies are used to detect hemoglobin in the stool. The sensitivity and specificity of 1-time FIT are 79% to 80% and 94%, respectively, for the detection of CRC, with sensitivity improving with successive testing.7,8 Annual FIT is recognized as a tier 1 preferred screening method by the US Multi-Society Task Force on Colorectal Cancer.7,9 Programs that mail FIT kits to eligible patients outside of physician visits have been successfully implemented in health care systems.10,11
The VACHS designed and implemented a mailed FIT program using existing infrastructure and staffing.
Program Description
A team of local stakeholders comprised of VACHS leadership, primary care, nursing, and gastroenterology staff, as well as representatives from laboratory, informatics, mail services, and group practice management, was established to execute the project. The team met monthly to plan the project.
The team developed a dataset consisting of patients aged 45 to 75 years who were at average risk for CRC and due for CRC screening. Patients were defined as due for CRC screening if they had not had a colonoscopy in the previous 9 years or a FIT or fecal occult blood test in the previous 11 months. Average risk for CRC was defined by excluding patients with associated diagnosis codes for CRC, colectomy, inflammatory bowel disease, and anemia. The program also excluded patients with diagnosis codes associated with dementia, deferring discussions about cancer screening to their primary care practitioners (PCPs). Patients with invalid mailing addresses were also excluded, as well as those whose PCPs had indicated in the electronic health record that the patient received CRC screening outside the US Department of Veterans Affairs (VA) system.
Letter Templates
Two patient letter electronic health record templates were developed. The first was a primer letter, which was mailed to patients 2 to 3 weeks before the mailed FIT kit as an introduction to the program.12 The purpose of the primer letter was to give advance notice to patients that they could expect a FIT kit to arrive in the mail. The goal was to prepare patients to complete FIT when the kit arrived and prompt them to call the VA to opt out of the mailed FIT program if they were up to date with CRC screening or if they had a condition which made them at high risk for CRC.
The second FIT letter arrived with the FIT kit, introduced FIT and described the importance of CRC screening. The letter detailed instructions for completing FIT and automatically created a FIT order. It also included a list of common conditions that may exclude patients, with a recommendation for patients to contact their medical team if they felt they were not candidates for FIT.
Staff Education
A previous VACHS pilot project demonstrated the success of a mailed FIT program to increase FIT use. Implemented as part of the pilot program, staff education consisted of a session for clinicians about the role of FIT in CRC screening and an all-staff education session. An additional education session about CRC and FIT for all staff was repeated with the program launch.
Program Launch
The mailed FIT program was introduced during a VACHS primary care all-staff meeting. After the meeting, each patient aligned care team (PACT) received an encrypted email that included a list of the patients on their team who were candidates for the program, a patient-facing FIT instruction sheet, detailed instructions on how to send the FIT primer letter, and a FIT package consisting of the labeled FIT kit, FIT letter, and patient instruction sheet. A reminder letter was sent to each patient 3 weeks after the FIT package was mailed. The patient lists were populated into a shared, encrypted Microsoft Teams folder that was edited in real time by PACT teams and viewed by VACHS leadership to track progress.
Program Metrics
At program launch, the VACHS had 4642 patients due for CRC screening who were eligible for the mailed FIT program. On March 7, 2023, the data consisting of FIT tests ordered between December 2022 and May 2023—3 months before and after the launch of the program—were reviewed and categorized. In the 3 months before program launch, 1528 FIT were ordered and 714 were returned (46.7%). In the 3 months after the launch of the program, 4383 FIT were ordered and 1712 were returned (39.1%) (Figure). Test orders increased 287% from the preintervention to the postintervention period. The mean (SD) number of monthly FIT tests prelaunch was 509 (32.7), which increased to 1461 (331.6) postlaunch.
At the VACHS, 61.4% of patients aged 45 to 75 years were up to date with CRC screening before the program launch. In the 3 months after program launch, the rate increased to 63.8% among patients aged 45 to 75 years, the highest rate in our Veterans Integrated Services Network and exceeding the VA national average CRC screening rate, according to unpublished VA Monthly Management Report data.
In the 3 months following the program launch, 139 FIT kits tested positive for potential CRC. Of these, 79 (56.8%) patients had completed a diagnostic colonoscopy. PACT PCPs and nurses received reports on patients with positive FIT tests and those with no colonoscopy scheduled or completed and were asked to follow up.
Discussion
Through a proactive, population-based CRC screening program centered on mailed FIT kits outside of the traditional patient visit, the VACHS increased the use of FIT and rates of CRC screening. The numbers of FIT kits ordered and completed substantially increased in the 3 months after program launch.
Compared to mailed FIT programs described in the literature that rely on centralized processes in that a separate team operates the mailed FIT program for the entire organization, this program used existing PACT infrastructure and staff.10,11 This strategy allowed VACHS to design and implement the program in several months. Not needing to hire new staff or create a central team for the sole purpose of implementing the program allowed us to save on any organizational funding and efforts that would have accompanied the additional staff. The program described in this article may be more attainable for primary care practices or smaller health systems that do not have the capacity for the creation of a centralized process.
Limitations
Although the total number of FIT completions substantially increased during the program, the rate of FIT completion during the mailed FIT program was lower than the rate of completion prior to program launch. This decreased rate of FIT kit completion may be related to separation from a patient visit and potential loss of real-time education with a clinician. The program’s decentralized design increased the existing workload for primary care staff, and as a result, consideration must be given to local staffing levels. Additionally, the report of eligible patients depended on diagnosis codes and may have captured patients with higher-than-average risk of CRC, such as patients with prior history of adenomatous polyps, family history of CRC, or other medical or genetic conditions. We attempted to mitigate this by including a list of conditions that would exclude patients from FIT eligibility in the FIT letter and giving them the option to opt out.
Conclusions
CRC screening rates improved following implementation of a primary care team-centered quality improvement process to proactively identify patients appropriate for FIT and mail them FIT kits. This project highlights that population-health interventions around CRC screening via use of FIT can be successful within a primary care patient-centered medical home model, considering the increases in both CRC screening rates and increase in FIT tests ordered.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 29, 2024. Accessed June 11, 2024. https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html
2. Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-884. doi:10.1001/jamaoncol.2021.0884
3. Mazidimoradi A, Tiznobaik A, Salehiniya H. Impact of the COVID-19 pandemic on colorectal cancer screening: a systematic review. J Gastrointest Cancer. 2022;53(3):730-744. doi:10.1007/s12029-021-00679-x
4. Adams MA, Kurlander JE, Gao Y, Yankey N, Saini SD. Impact of coronavirus disease 2019 on screening colonoscopy utilization in a large integrated health system. Gastroenterology. 2022;162(7):2098-2100.e2. doi:10.1053/j.gastro.2022.02.034
5. Sundaram S, Olson S, Sharma P, Rajendra S. A review of the impact of the COVID-19 pandemic on colorectal cancer screening: implications and solutions. Pathogens. 2021;10(11):558. doi:10.3390/pathogens10111508
6. US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977. doi:10.1001/jama.2021.6238
7. Robertson DJ, Lee JK, Boland CR, et al. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2017;85(1):2-21.e3. doi:10.1016/j.gie.2016.09.025
8. Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160(3):171. doi:10.7326/M13-1484
9. Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153(1):307-323. doi:10.1053/j.gastro.2017.05.013
10. Deeds SA, Moore CB, Gunnink EJ, et al. Implementation of a mailed faecal immunochemical test programme for colorectal cancer screening among veterans. BMJ Open Qual. 2022;11(4):e001927. doi:10.1136/bmjoq-2022-001927
11. Selby K, Jensen CD, Levin TR, et al. Program components and results from an organized colorectal cancer screening program using annual fecal immunochemical testing. Clin Gastroenterol Hepatol. 2022;20(1):145-152. doi:10.1016/j.cgh.2020.09.042
12. Deeds S, Liu T, Schuttner L, et al. A postcard primer prior to mailed fecal immunochemical test among veterans: a randomized controlled trial. J Gen Intern Med. 2023:38(14):3235-3241. doi:10.1007/s11606-023-08248-7
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 29, 2024. Accessed June 11, 2024. https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html
2. Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-884. doi:10.1001/jamaoncol.2021.0884
3. Mazidimoradi A, Tiznobaik A, Salehiniya H. Impact of the COVID-19 pandemic on colorectal cancer screening: a systematic review. J Gastrointest Cancer. 2022;53(3):730-744. doi:10.1007/s12029-021-00679-x
4. Adams MA, Kurlander JE, Gao Y, Yankey N, Saini SD. Impact of coronavirus disease 2019 on screening colonoscopy utilization in a large integrated health system. Gastroenterology. 2022;162(7):2098-2100.e2. doi:10.1053/j.gastro.2022.02.034
5. Sundaram S, Olson S, Sharma P, Rajendra S. A review of the impact of the COVID-19 pandemic on colorectal cancer screening: implications and solutions. Pathogens. 2021;10(11):558. doi:10.3390/pathogens10111508
6. US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977. doi:10.1001/jama.2021.6238
7. Robertson DJ, Lee JK, Boland CR, et al. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2017;85(1):2-21.e3. doi:10.1016/j.gie.2016.09.025
8. Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160(3):171. doi:10.7326/M13-1484
9. Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153(1):307-323. doi:10.1053/j.gastro.2017.05.013
10. Deeds SA, Moore CB, Gunnink EJ, et al. Implementation of a mailed faecal immunochemical test programme for colorectal cancer screening among veterans. BMJ Open Qual. 2022;11(4):e001927. doi:10.1136/bmjoq-2022-001927
11. Selby K, Jensen CD, Levin TR, et al. Program components and results from an organized colorectal cancer screening program using annual fecal immunochemical testing. Clin Gastroenterol Hepatol. 2022;20(1):145-152. doi:10.1016/j.cgh.2020.09.042
12. Deeds S, Liu T, Schuttner L, et al. A postcard primer prior to mailed fecal immunochemical test among veterans: a randomized controlled trial. J Gen Intern Med. 2023:38(14):3235-3241. doi:10.1007/s11606-023-08248-7
GLP-1s May Improve Colon Cancer Outcomes
Treatment with a GLP-1 receptor agonist (RA) may offer a survival advantage in patients with colon cancer and obesity.
In a real-world analysis of nearly 7000 patients with colon cancer, those taking a GLP-1 RA were less than half as likely to die within 5 years compared with those who weren’t on a GLP-1 drug.
The association between GLP-1 exposure and lower 5–year mortality in colon cancer was “robust” and appeared to be concentrated in patients with severe obesity (BMI ≥ 35), lead investigator Raphael E. Cuomo, PhD, with University of California San Diego, told this news organization.
The apparent protective effect “persisted after controlling for differences in disease severity and demographics, as well as differences in circulating carcinoembryonic antigen, a biomarker of disease aggressiveness,” Cuomo said.
The study was published online in Cancer Investigation.
Effects Beyond Glucose-Lowering
Colon cancer remains a major global cause of cancer-related deaths, and obesity is both a risk factor and a driver of worse outcomes.
Beyond regulating blood sugar, GLP-1 drugs reduce systemic inflammation, improve insulin sensitivity, and promote weight loss. Prior preclinical work has also suggested they may prevent cancer cell growth, trigger cancer cell death, and reshape the tumor microenvironment.
To investigate further, Cuomo analyzed electronic health records of 6871 patients diagnosed with primary colon cancer before 2019 — of which 103 had at least 1 documented prescription for a GLP-1 drug within 5 years of diagnosis.
Five–year mortality was significantly lower in GLP-1 RA users than in nonusers (15.5% vs 37.1%; P < .001). A significant reduction in 5–year mortality among GLP-1 RA users was evident in an unadjusted model (odds ratio [OR], 0.38; P < .001) and persisted in fully adjusted models (OR, 0.28; P < .001).
When stratified by BMI, the odds of 5-year mortality with GLP-1 use was reduced only in patients with Class II obesity (BMI ≥ 35: fully adjusted hazard ratio [HR], 0.051; P = .004). In this group, fully adjusted hazard ratios suggested markedly lower risk for death (HR, 0.07; P = .009).
Beyond mortality, GLP-1 users also experienced fewer late cardiovascular events and had fewer markers of advanced colon cancer progression in the final months of follow-up, “which suggests that GLP-1 drugs exert benefits through both oncologic and cardiometabolic pathways,” Cuomo told this news organization.
Intriguing and Promising — but Further Studies Needed
“To further study the potential of GLP-1 therapy as an adjunct to standard care in colon cancer, randomized trials should be conducted with stratification by BMI, diabetes status, and disease severity, with endpoints spanning overall and cancerspecific survival and major cardiovascular events,” Cuomo said.
“We also need prospective translational studies integrating dosing/timing, adherence, tumor genomics, and serial biomarkers (including ctDNA and metabolic panels) to elucidate mechanisms, assess the role of adiposity and insulin resistance, and identify the patient subgroups most likely to benefit,” he noted.
For now, GLP1 medications are an option in “eligible colon cancer patients with severe obesity or diabetes who meet standard metabolic indications,” Cuomo told this news organization.
Commenting on this study for this news organization, David Greenwald, MD, director of Clinical Gastroenterology and Endoscopy at Icahn School of Medicine at Mount Sinai Hospital in New York City, noted “other studies have showed a lower risk of developing colorectal cancer in the first place and then improved survival.”
Greenwald cited a recent study that found people with diabetes who took GLP-1 RAs had a 44% lower risk of developing colorectal cancer than those who took insulin, and a 25% lower risk than those who took metformin.
The effects of GLP-1s in colon cancer are “very intriguing and very promising but more research is needed to confirm whether this is really true and the mechanisms behind it,” said Greenwald.
In terms of the lowering risk of developing colorectal cancer, “probably first and foremost is that the drugs are really effective in promoting weight loss. And if you can reduce obesity in the population, you do all sorts of good things — reduce diabetes, reduce heart disease, and maybe reduce colorectal cancer,” Greenwald said.
This study had no specific funding. Cuomo and Greenwald had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Treatment with a GLP-1 receptor agonist (RA) may offer a survival advantage in patients with colon cancer and obesity.
In a real-world analysis of nearly 7000 patients with colon cancer, those taking a GLP-1 RA were less than half as likely to die within 5 years compared with those who weren’t on a GLP-1 drug.
The association between GLP-1 exposure and lower 5–year mortality in colon cancer was “robust” and appeared to be concentrated in patients with severe obesity (BMI ≥ 35), lead investigator Raphael E. Cuomo, PhD, with University of California San Diego, told this news organization.
The apparent protective effect “persisted after controlling for differences in disease severity and demographics, as well as differences in circulating carcinoembryonic antigen, a biomarker of disease aggressiveness,” Cuomo said.
The study was published online in Cancer Investigation.
Effects Beyond Glucose-Lowering
Colon cancer remains a major global cause of cancer-related deaths, and obesity is both a risk factor and a driver of worse outcomes.
Beyond regulating blood sugar, GLP-1 drugs reduce systemic inflammation, improve insulin sensitivity, and promote weight loss. Prior preclinical work has also suggested they may prevent cancer cell growth, trigger cancer cell death, and reshape the tumor microenvironment.
To investigate further, Cuomo analyzed electronic health records of 6871 patients diagnosed with primary colon cancer before 2019 — of which 103 had at least 1 documented prescription for a GLP-1 drug within 5 years of diagnosis.
Five–year mortality was significantly lower in GLP-1 RA users than in nonusers (15.5% vs 37.1%; P < .001). A significant reduction in 5–year mortality among GLP-1 RA users was evident in an unadjusted model (odds ratio [OR], 0.38; P < .001) and persisted in fully adjusted models (OR, 0.28; P < .001).
When stratified by BMI, the odds of 5-year mortality with GLP-1 use was reduced only in patients with Class II obesity (BMI ≥ 35: fully adjusted hazard ratio [HR], 0.051; P = .004). In this group, fully adjusted hazard ratios suggested markedly lower risk for death (HR, 0.07; P = .009).
Beyond mortality, GLP-1 users also experienced fewer late cardiovascular events and had fewer markers of advanced colon cancer progression in the final months of follow-up, “which suggests that GLP-1 drugs exert benefits through both oncologic and cardiometabolic pathways,” Cuomo told this news organization.
Intriguing and Promising — but Further Studies Needed
“To further study the potential of GLP-1 therapy as an adjunct to standard care in colon cancer, randomized trials should be conducted with stratification by BMI, diabetes status, and disease severity, with endpoints spanning overall and cancerspecific survival and major cardiovascular events,” Cuomo said.
“We also need prospective translational studies integrating dosing/timing, adherence, tumor genomics, and serial biomarkers (including ctDNA and metabolic panels) to elucidate mechanisms, assess the role of adiposity and insulin resistance, and identify the patient subgroups most likely to benefit,” he noted.
For now, GLP1 medications are an option in “eligible colon cancer patients with severe obesity or diabetes who meet standard metabolic indications,” Cuomo told this news organization.
Commenting on this study for this news organization, David Greenwald, MD, director of Clinical Gastroenterology and Endoscopy at Icahn School of Medicine at Mount Sinai Hospital in New York City, noted “other studies have showed a lower risk of developing colorectal cancer in the first place and then improved survival.”
Greenwald cited a recent study that found people with diabetes who took GLP-1 RAs had a 44% lower risk of developing colorectal cancer than those who took insulin, and a 25% lower risk than those who took metformin.
The effects of GLP-1s in colon cancer are “very intriguing and very promising but more research is needed to confirm whether this is really true and the mechanisms behind it,” said Greenwald.
In terms of the lowering risk of developing colorectal cancer, “probably first and foremost is that the drugs are really effective in promoting weight loss. And if you can reduce obesity in the population, you do all sorts of good things — reduce diabetes, reduce heart disease, and maybe reduce colorectal cancer,” Greenwald said.
This study had no specific funding. Cuomo and Greenwald had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Treatment with a GLP-1 receptor agonist (RA) may offer a survival advantage in patients with colon cancer and obesity.
In a real-world analysis of nearly 7000 patients with colon cancer, those taking a GLP-1 RA were less than half as likely to die within 5 years compared with those who weren’t on a GLP-1 drug.
The association between GLP-1 exposure and lower 5–year mortality in colon cancer was “robust” and appeared to be concentrated in patients with severe obesity (BMI ≥ 35), lead investigator Raphael E. Cuomo, PhD, with University of California San Diego, told this news organization.
The apparent protective effect “persisted after controlling for differences in disease severity and demographics, as well as differences in circulating carcinoembryonic antigen, a biomarker of disease aggressiveness,” Cuomo said.
The study was published online in Cancer Investigation.
Effects Beyond Glucose-Lowering
Colon cancer remains a major global cause of cancer-related deaths, and obesity is both a risk factor and a driver of worse outcomes.
Beyond regulating blood sugar, GLP-1 drugs reduce systemic inflammation, improve insulin sensitivity, and promote weight loss. Prior preclinical work has also suggested they may prevent cancer cell growth, trigger cancer cell death, and reshape the tumor microenvironment.
To investigate further, Cuomo analyzed electronic health records of 6871 patients diagnosed with primary colon cancer before 2019 — of which 103 had at least 1 documented prescription for a GLP-1 drug within 5 years of diagnosis.
Five–year mortality was significantly lower in GLP-1 RA users than in nonusers (15.5% vs 37.1%; P < .001). A significant reduction in 5–year mortality among GLP-1 RA users was evident in an unadjusted model (odds ratio [OR], 0.38; P < .001) and persisted in fully adjusted models (OR, 0.28; P < .001).
When stratified by BMI, the odds of 5-year mortality with GLP-1 use was reduced only in patients with Class II obesity (BMI ≥ 35: fully adjusted hazard ratio [HR], 0.051; P = .004). In this group, fully adjusted hazard ratios suggested markedly lower risk for death (HR, 0.07; P = .009).
Beyond mortality, GLP-1 users also experienced fewer late cardiovascular events and had fewer markers of advanced colon cancer progression in the final months of follow-up, “which suggests that GLP-1 drugs exert benefits through both oncologic and cardiometabolic pathways,” Cuomo told this news organization.
Intriguing and Promising — but Further Studies Needed
“To further study the potential of GLP-1 therapy as an adjunct to standard care in colon cancer, randomized trials should be conducted with stratification by BMI, diabetes status, and disease severity, with endpoints spanning overall and cancerspecific survival and major cardiovascular events,” Cuomo said.
“We also need prospective translational studies integrating dosing/timing, adherence, tumor genomics, and serial biomarkers (including ctDNA and metabolic panels) to elucidate mechanisms, assess the role of adiposity and insulin resistance, and identify the patient subgroups most likely to benefit,” he noted.
For now, GLP1 medications are an option in “eligible colon cancer patients with severe obesity or diabetes who meet standard metabolic indications,” Cuomo told this news organization.
Commenting on this study for this news organization, David Greenwald, MD, director of Clinical Gastroenterology and Endoscopy at Icahn School of Medicine at Mount Sinai Hospital in New York City, noted “other studies have showed a lower risk of developing colorectal cancer in the first place and then improved survival.”
Greenwald cited a recent study that found people with diabetes who took GLP-1 RAs had a 44% lower risk of developing colorectal cancer than those who took insulin, and a 25% lower risk than those who took metformin.
The effects of GLP-1s in colon cancer are “very intriguing and very promising but more research is needed to confirm whether this is really true and the mechanisms behind it,” said Greenwald.
In terms of the lowering risk of developing colorectal cancer, “probably first and foremost is that the drugs are really effective in promoting weight loss. And if you can reduce obesity in the population, you do all sorts of good things — reduce diabetes, reduce heart disease, and maybe reduce colorectal cancer,” Greenwald said.
This study had no specific funding. Cuomo and Greenwald had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM CANCER INVESTIGATION
Does This Bacterial Toxin Drive Early CRC Risk?
Recent studies have cited an alarming increase in early-onset colorectal cancer (CRC) rates, raising concern among gastroenterologists, public health experts, and patients alike. Approximately 10% of CRC cases now occur in those under age 50, and that proportion continues to grow. Between 2000 and 2016, colon cancer rose by 13% and rectal cancer by 16% among those aged 40–49.
According to recently published data from the Surveillance, Epidemiology and End Results Program, between 2019 and 2022, CRC incidence among patients aged 45–49 rose by approximately 12% per year.
A Potential Bacterial Connection
What accounts for this disturbing spike? A research group from the University of California, San Diego, may have uncovered part of the answer.
In their study of 981 CRC genomes, most carried mutations suggestive of prior exposure to colibactin, a toxin produced by certain Escherichia coli (E coli) strains. Patients with extremely early-onset CRC (aged < 40 years) were 3 times more likely to have colibactin-suggestive mutations than patients older than 70. Crucially, colonic exposure to colibactin was linked to an adenomatous polyposis coli driver mutation.
These findings suggest that colibactin-induced injury in the gut microbiome may accelerate cancer development in some individuals. Environmental factors may contribute to the rise in early-onset CRC as well, such as consuming red meats, carcinogens from grilling, and processed meats and other highly processed foods; low fiber intake; lack of fruits and vegetables; drinking alcohol; lack of exercise; obesity; and colibactin exposure.
In this video, we will take a closer look at how E coli and colibactin may increase CRC risk.
Bacteria’s Cancer-Causing Properties
The idea that bacteria has cancer-causing properties isn’t new. In the 1970s, researchers linked Streptococcus bovis type 1 (now called Streptococcus gallolyticus) to CRC in a subset of patients with bacterial endocarditis stemming from right-sided colon cancer. Similarly, Helicobacter pylori infection has long been associated with increased gastric cancer risk.
Today, E coli infection is emerging as another possible contributor to CRC, especially via certain pathogenic strains containing the polyketide synthase (pks) genomic island, which encodes the colibactin and is sometimes present in the colon mucosa of patients with CRC.
Colibactin and DNA Damage
Colibactin-producing pks+ E coli strains can cause DNA double-strand breaks, one pathway to carcinogenesis. In animal studies, pks+ E coli strains have been linked to both increased risk for CRC and CRC progression.
In an important study published in Nature, Pleguezuelos-Manzano and colleagues repeatedly exposed intestinal organoids to pks+ E coli over 5 months and then performed whole genome sequencing. The result was a concerning potential for short insertions and deletions and single–base substitutions.
The authors concluded that their “study describes the distinct mutational signature in colorectal cancer and implies that the underlying mutational process results directly from past exposure to bacteria carrying the colibactin-producing pks pathogenicity island.”
Other E coli virulence factors may also contribute. For example, alpha-hemolysin may downregulate DNA mismatch repair proteins. In other words, E coli is probably just a contributing factor for the development of CRC, not the sole cause.
Biofilms and Inflammation
Previous studies have associated dense bacterial biofilms, particularly antibiotic-resistant strains, with CRC. This raises the possibility that widespread antibiotic overuse could predispose certain individuals to CRC development.
Biofilms normally separate the colon mucosal epithelium from bacteria and are essential for protecting against inflammation. In a 2018 study in Science, Dejea and colleagues concluded that “tumor-prone mice colonized with E coli (expressing colibactin), and enterotoxigenic B fragilis showed increased interleukin-17 in the colon and DNA damage in colonic epithelium with faster tumor onset and greater mortality, compared to mice with either bacteria strain alone. These data suggest an unexpected link between early neoplasia of the colon and tumorigenic bacteria.”
Additional research revealed that E coli can create a pro-carcinogenic environment by stimulating mucosal inflammation, hindering DNA and mismatch repair mechanisms, and altering immune responses.
Dysbiosis and Diet
Colibactin can also drive dysbiosis and imbalance in bacteria in the colon, which fuels inflammation and disrupts mucosal barrier integrity. This creates a vicious cycle in which chronic inflammation can further drive additional mucus deterioration and dysbiosis.
In mouse models where the colon mucosal barrier is damaged with dextrin sulfate sodium (DSS), pks+ E coli gains better access to colon epithelium, causes injury, and can even lead to chronic colitis. Colibactin can also hinder epithelial recovery after DSS treatment.
Diet plays a central role in this process. Low fiber consumption can disrupt the barrier between the colon mucus layer and the colon’s exterior layer where bacteria live. A traditional Western diet may bolster bacteria that degrade the mucus layer when the bacteria consume the glycosylated portion as an energy source.
Fortunately, diet is modifiable. High–fiber diets (ideally 25-30 g/d) boost short–chain fatty acids in the colon. This is important because short-chain fatty acids can decrease intercellular pH and impede Enterobacteriaceae replication, yet another reason why we should encourage patients to eat a diet high in vegetables, fruits, and [green] salads.
Two Types of Bacterial Drivers
There appear to be two broad types of bacteria associated with CRC development. It’s been hypothesized that there are “driver” bacteria that might initiate the development of CRC, possibly by creating oxidative stress and causing DNA breaks. Several potential pathogenic bacteria have been identified, including E coli, Enterococcus faecalis, and Bacteroides fragilis. Unfortunately, there are also bacteria such as Fusobacterium species and Streptococcus gallolyticus with the potential to alter intestinal permeability, resulting in downstream effects that can allow colon cancers to expand. Fusobacterium species and Streptococcus gallolyticus have the potential to cause DNA double–strand breaks in the intestine, which can produce chromosomal precariousness.
These secondary bacteria can also lead to DNA epigenetic changes and gene mutations. However, it should be emphasized that “the direct causation of imprinted DNA changes resulting from a direct interaction between bacteria and host cells is not so far established.”
E coli produces compounds called cyclomodulins, which can cause DNA breaks and potentially trigger cell cycle arrest and even cell death through activation of the DNA damage checkpoint pathway. The DNA damage checkpoint pathway is a cellular signaling network that helps detect DNA lesions and allows for genetic stability by stopping growth to allow for repair and simulating cell survival or apoptosis. A key cyclomodulin that E coli makes is colibactin, produced by the pks locus. Other cyclomodulins include cytolethal distending toxin, cytotoxic necrotizing factor, and cycle-inhibiting factor.
Previous research has shown that E coli is the only culturable bacteria found near CRC. A groundbreaking 1998 study employing PCR technology found E coli in 60% of colon polyp adenomas and an alarming 77% of CRC biopsies.
E coli’s capability to downregulate essential DNA mismatch repair proteins has been implicated in colorectal carcinogenesis. Interestingly, when the genetic region responsible for producing colibactin is deleted in animals, the bacteria aren’t able to promote cancer.
Mechanistically, colibactin causes double-stranded DNA breaks, eukaryotic cell cycle arrest, and chromosome abnormalities. It also alkylates DNA. This occurs when the cyclopropane ring of colibactin interacts with the N3 position of adenine in DNA, forming a covalent bond and creating a DNA adduct. DNA adducts occur when a chemical moiety from an environmental or dietary source binds to DNA base. Colibactin can cause DNA interstrand cross-links to form via alkalization of adenine residues on opposing DNA strands, a crucial step in DNA damage. DNA adducts can occur through carcinogens in N-nitroso compounds, such as in processed meats and in polycyclic aromatic hydrocarbons found in cigarette smoke. Colibactin-induced damage may also stimulate the senescence–associated secretory phenotype pathway, increasing proinflammatory cytokines.
E coli and Inflammatory Bowel Disease
E coli, the primary colibactin producer in the human intestinal microbiome, is found at higher bacterial percentages in the microbiomes of patients with inflammatory bowel disease (IBD). In a study by Dubinsky and colleagues, “the medium relative levels of colibactin–encoding E. coli were about threefold higher in IBD.”
Researchers have also postulated that antibiotics and microbiome dysbiosis may create conditions that allow colibactin–producing bacteria to overpopulate.
Future Directions
Not every patient with CRC carries a colorectal mutational signature, but these findings underscore the need for continued vigilance and prevention.
From a public health standpoint, our advice remains consistent: Promote high-fiber diets with more vegetables and less red meat; avoid highly processed foods; avoid alcohol; encourage exercise; and address overweight and obesity. Our goal is to create the best possible colon environment to prevent DNA damage from bacterial and environmental carcinogens.
In the future, we need more research to clarify exactly how E coli and colibactin increase early–onset CRC risk and whether antibiotics and dysbiosis facilitate their ability to damage the DNA of colon mucosa. It’s still unclear why younger patients are at greater risk. In time, we may be able to screen for colibactin–producing bacteria such as E coli and manipulate the fecal microbiome to prevent damage.
A recent mouse study in Nature by Jans and colleagues suggests it might be possible to block bacterial adhesion and hopefully mitigate damage caused by colibactin. With continued work, colibactin–targeted strategies could become a part of CRC prevention.
Benjamin H. Levy III, MD, is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who gave a TEDx Talk about building health education campaigns using music and concerts, organizes "Tune It Up: A Concert To Raise Colorectal Cancer Awareness" with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee.
A version of this article first appeared on Medscape.com.
Recent studies have cited an alarming increase in early-onset colorectal cancer (CRC) rates, raising concern among gastroenterologists, public health experts, and patients alike. Approximately 10% of CRC cases now occur in those under age 50, and that proportion continues to grow. Between 2000 and 2016, colon cancer rose by 13% and rectal cancer by 16% among those aged 40–49.
According to recently published data from the Surveillance, Epidemiology and End Results Program, between 2019 and 2022, CRC incidence among patients aged 45–49 rose by approximately 12% per year.
A Potential Bacterial Connection
What accounts for this disturbing spike? A research group from the University of California, San Diego, may have uncovered part of the answer.
In their study of 981 CRC genomes, most carried mutations suggestive of prior exposure to colibactin, a toxin produced by certain Escherichia coli (E coli) strains. Patients with extremely early-onset CRC (aged < 40 years) were 3 times more likely to have colibactin-suggestive mutations than patients older than 70. Crucially, colonic exposure to colibactin was linked to an adenomatous polyposis coli driver mutation.
These findings suggest that colibactin-induced injury in the gut microbiome may accelerate cancer development in some individuals. Environmental factors may contribute to the rise in early-onset CRC as well, such as consuming red meats, carcinogens from grilling, and processed meats and other highly processed foods; low fiber intake; lack of fruits and vegetables; drinking alcohol; lack of exercise; obesity; and colibactin exposure.
In this video, we will take a closer look at how E coli and colibactin may increase CRC risk.
Bacteria’s Cancer-Causing Properties
The idea that bacteria has cancer-causing properties isn’t new. In the 1970s, researchers linked Streptococcus bovis type 1 (now called Streptococcus gallolyticus) to CRC in a subset of patients with bacterial endocarditis stemming from right-sided colon cancer. Similarly, Helicobacter pylori infection has long been associated with increased gastric cancer risk.
Today, E coli infection is emerging as another possible contributor to CRC, especially via certain pathogenic strains containing the polyketide synthase (pks) genomic island, which encodes the colibactin and is sometimes present in the colon mucosa of patients with CRC.
Colibactin and DNA Damage
Colibactin-producing pks+ E coli strains can cause DNA double-strand breaks, one pathway to carcinogenesis. In animal studies, pks+ E coli strains have been linked to both increased risk for CRC and CRC progression.
In an important study published in Nature, Pleguezuelos-Manzano and colleagues repeatedly exposed intestinal organoids to pks+ E coli over 5 months and then performed whole genome sequencing. The result was a concerning potential for short insertions and deletions and single–base substitutions.
The authors concluded that their “study describes the distinct mutational signature in colorectal cancer and implies that the underlying mutational process results directly from past exposure to bacteria carrying the colibactin-producing pks pathogenicity island.”
Other E coli virulence factors may also contribute. For example, alpha-hemolysin may downregulate DNA mismatch repair proteins. In other words, E coli is probably just a contributing factor for the development of CRC, not the sole cause.
Biofilms and Inflammation
Previous studies have associated dense bacterial biofilms, particularly antibiotic-resistant strains, with CRC. This raises the possibility that widespread antibiotic overuse could predispose certain individuals to CRC development.
Biofilms normally separate the colon mucosal epithelium from bacteria and are essential for protecting against inflammation. In a 2018 study in Science, Dejea and colleagues concluded that “tumor-prone mice colonized with E coli (expressing colibactin), and enterotoxigenic B fragilis showed increased interleukin-17 in the colon and DNA damage in colonic epithelium with faster tumor onset and greater mortality, compared to mice with either bacteria strain alone. These data suggest an unexpected link between early neoplasia of the colon and tumorigenic bacteria.”
Additional research revealed that E coli can create a pro-carcinogenic environment by stimulating mucosal inflammation, hindering DNA and mismatch repair mechanisms, and altering immune responses.
Dysbiosis and Diet
Colibactin can also drive dysbiosis and imbalance in bacteria in the colon, which fuels inflammation and disrupts mucosal barrier integrity. This creates a vicious cycle in which chronic inflammation can further drive additional mucus deterioration and dysbiosis.
In mouse models where the colon mucosal barrier is damaged with dextrin sulfate sodium (DSS), pks+ E coli gains better access to colon epithelium, causes injury, and can even lead to chronic colitis. Colibactin can also hinder epithelial recovery after DSS treatment.
Diet plays a central role in this process. Low fiber consumption can disrupt the barrier between the colon mucus layer and the colon’s exterior layer where bacteria live. A traditional Western diet may bolster bacteria that degrade the mucus layer when the bacteria consume the glycosylated portion as an energy source.
Fortunately, diet is modifiable. High–fiber diets (ideally 25-30 g/d) boost short–chain fatty acids in the colon. This is important because short-chain fatty acids can decrease intercellular pH and impede Enterobacteriaceae replication, yet another reason why we should encourage patients to eat a diet high in vegetables, fruits, and [green] salads.
Two Types of Bacterial Drivers
There appear to be two broad types of bacteria associated with CRC development. It’s been hypothesized that there are “driver” bacteria that might initiate the development of CRC, possibly by creating oxidative stress and causing DNA breaks. Several potential pathogenic bacteria have been identified, including E coli, Enterococcus faecalis, and Bacteroides fragilis. Unfortunately, there are also bacteria such as Fusobacterium species and Streptococcus gallolyticus with the potential to alter intestinal permeability, resulting in downstream effects that can allow colon cancers to expand. Fusobacterium species and Streptococcus gallolyticus have the potential to cause DNA double–strand breaks in the intestine, which can produce chromosomal precariousness.
These secondary bacteria can also lead to DNA epigenetic changes and gene mutations. However, it should be emphasized that “the direct causation of imprinted DNA changes resulting from a direct interaction between bacteria and host cells is not so far established.”
E coli produces compounds called cyclomodulins, which can cause DNA breaks and potentially trigger cell cycle arrest and even cell death through activation of the DNA damage checkpoint pathway. The DNA damage checkpoint pathway is a cellular signaling network that helps detect DNA lesions and allows for genetic stability by stopping growth to allow for repair and simulating cell survival or apoptosis. A key cyclomodulin that E coli makes is colibactin, produced by the pks locus. Other cyclomodulins include cytolethal distending toxin, cytotoxic necrotizing factor, and cycle-inhibiting factor.
Previous research has shown that E coli is the only culturable bacteria found near CRC. A groundbreaking 1998 study employing PCR technology found E coli in 60% of colon polyp adenomas and an alarming 77% of CRC biopsies.
E coli’s capability to downregulate essential DNA mismatch repair proteins has been implicated in colorectal carcinogenesis. Interestingly, when the genetic region responsible for producing colibactin is deleted in animals, the bacteria aren’t able to promote cancer.
Mechanistically, colibactin causes double-stranded DNA breaks, eukaryotic cell cycle arrest, and chromosome abnormalities. It also alkylates DNA. This occurs when the cyclopropane ring of colibactin interacts with the N3 position of adenine in DNA, forming a covalent bond and creating a DNA adduct. DNA adducts occur when a chemical moiety from an environmental or dietary source binds to DNA base. Colibactin can cause DNA interstrand cross-links to form via alkalization of adenine residues on opposing DNA strands, a crucial step in DNA damage. DNA adducts can occur through carcinogens in N-nitroso compounds, such as in processed meats and in polycyclic aromatic hydrocarbons found in cigarette smoke. Colibactin-induced damage may also stimulate the senescence–associated secretory phenotype pathway, increasing proinflammatory cytokines.
E coli and Inflammatory Bowel Disease
E coli, the primary colibactin producer in the human intestinal microbiome, is found at higher bacterial percentages in the microbiomes of patients with inflammatory bowel disease (IBD). In a study by Dubinsky and colleagues, “the medium relative levels of colibactin–encoding E. coli were about threefold higher in IBD.”
Researchers have also postulated that antibiotics and microbiome dysbiosis may create conditions that allow colibactin–producing bacteria to overpopulate.
Future Directions
Not every patient with CRC carries a colorectal mutational signature, but these findings underscore the need for continued vigilance and prevention.
From a public health standpoint, our advice remains consistent: Promote high-fiber diets with more vegetables and less red meat; avoid highly processed foods; avoid alcohol; encourage exercise; and address overweight and obesity. Our goal is to create the best possible colon environment to prevent DNA damage from bacterial and environmental carcinogens.
In the future, we need more research to clarify exactly how E coli and colibactin increase early–onset CRC risk and whether antibiotics and dysbiosis facilitate their ability to damage the DNA of colon mucosa. It’s still unclear why younger patients are at greater risk. In time, we may be able to screen for colibactin–producing bacteria such as E coli and manipulate the fecal microbiome to prevent damage.
A recent mouse study in Nature by Jans and colleagues suggests it might be possible to block bacterial adhesion and hopefully mitigate damage caused by colibactin. With continued work, colibactin–targeted strategies could become a part of CRC prevention.
Benjamin H. Levy III, MD, is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who gave a TEDx Talk about building health education campaigns using music and concerts, organizes "Tune It Up: A Concert To Raise Colorectal Cancer Awareness" with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee.
A version of this article first appeared on Medscape.com.
Recent studies have cited an alarming increase in early-onset colorectal cancer (CRC) rates, raising concern among gastroenterologists, public health experts, and patients alike. Approximately 10% of CRC cases now occur in those under age 50, and that proportion continues to grow. Between 2000 and 2016, colon cancer rose by 13% and rectal cancer by 16% among those aged 40–49.
According to recently published data from the Surveillance, Epidemiology and End Results Program, between 2019 and 2022, CRC incidence among patients aged 45–49 rose by approximately 12% per year.
A Potential Bacterial Connection
What accounts for this disturbing spike? A research group from the University of California, San Diego, may have uncovered part of the answer.
In their study of 981 CRC genomes, most carried mutations suggestive of prior exposure to colibactin, a toxin produced by certain Escherichia coli (E coli) strains. Patients with extremely early-onset CRC (aged < 40 years) were 3 times more likely to have colibactin-suggestive mutations than patients older than 70. Crucially, colonic exposure to colibactin was linked to an adenomatous polyposis coli driver mutation.
These findings suggest that colibactin-induced injury in the gut microbiome may accelerate cancer development in some individuals. Environmental factors may contribute to the rise in early-onset CRC as well, such as consuming red meats, carcinogens from grilling, and processed meats and other highly processed foods; low fiber intake; lack of fruits and vegetables; drinking alcohol; lack of exercise; obesity; and colibactin exposure.
In this video, we will take a closer look at how E coli and colibactin may increase CRC risk.
Bacteria’s Cancer-Causing Properties
The idea that bacteria has cancer-causing properties isn’t new. In the 1970s, researchers linked Streptococcus bovis type 1 (now called Streptococcus gallolyticus) to CRC in a subset of patients with bacterial endocarditis stemming from right-sided colon cancer. Similarly, Helicobacter pylori infection has long been associated with increased gastric cancer risk.
Today, E coli infection is emerging as another possible contributor to CRC, especially via certain pathogenic strains containing the polyketide synthase (pks) genomic island, which encodes the colibactin and is sometimes present in the colon mucosa of patients with CRC.
Colibactin and DNA Damage
Colibactin-producing pks+ E coli strains can cause DNA double-strand breaks, one pathway to carcinogenesis. In animal studies, pks+ E coli strains have been linked to both increased risk for CRC and CRC progression.
In an important study published in Nature, Pleguezuelos-Manzano and colleagues repeatedly exposed intestinal organoids to pks+ E coli over 5 months and then performed whole genome sequencing. The result was a concerning potential for short insertions and deletions and single–base substitutions.
The authors concluded that their “study describes the distinct mutational signature in colorectal cancer and implies that the underlying mutational process results directly from past exposure to bacteria carrying the colibactin-producing pks pathogenicity island.”
Other E coli virulence factors may also contribute. For example, alpha-hemolysin may downregulate DNA mismatch repair proteins. In other words, E coli is probably just a contributing factor for the development of CRC, not the sole cause.
Biofilms and Inflammation
Previous studies have associated dense bacterial biofilms, particularly antibiotic-resistant strains, with CRC. This raises the possibility that widespread antibiotic overuse could predispose certain individuals to CRC development.
Biofilms normally separate the colon mucosal epithelium from bacteria and are essential for protecting against inflammation. In a 2018 study in Science, Dejea and colleagues concluded that “tumor-prone mice colonized with E coli (expressing colibactin), and enterotoxigenic B fragilis showed increased interleukin-17 in the colon and DNA damage in colonic epithelium with faster tumor onset and greater mortality, compared to mice with either bacteria strain alone. These data suggest an unexpected link between early neoplasia of the colon and tumorigenic bacteria.”
Additional research revealed that E coli can create a pro-carcinogenic environment by stimulating mucosal inflammation, hindering DNA and mismatch repair mechanisms, and altering immune responses.
Dysbiosis and Diet
Colibactin can also drive dysbiosis and imbalance in bacteria in the colon, which fuels inflammation and disrupts mucosal barrier integrity. This creates a vicious cycle in which chronic inflammation can further drive additional mucus deterioration and dysbiosis.
In mouse models where the colon mucosal barrier is damaged with dextrin sulfate sodium (DSS), pks+ E coli gains better access to colon epithelium, causes injury, and can even lead to chronic colitis. Colibactin can also hinder epithelial recovery after DSS treatment.
Diet plays a central role in this process. Low fiber consumption can disrupt the barrier between the colon mucus layer and the colon’s exterior layer where bacteria live. A traditional Western diet may bolster bacteria that degrade the mucus layer when the bacteria consume the glycosylated portion as an energy source.
Fortunately, diet is modifiable. High–fiber diets (ideally 25-30 g/d) boost short–chain fatty acids in the colon. This is important because short-chain fatty acids can decrease intercellular pH and impede Enterobacteriaceae replication, yet another reason why we should encourage patients to eat a diet high in vegetables, fruits, and [green] salads.
Two Types of Bacterial Drivers
There appear to be two broad types of bacteria associated with CRC development. It’s been hypothesized that there are “driver” bacteria that might initiate the development of CRC, possibly by creating oxidative stress and causing DNA breaks. Several potential pathogenic bacteria have been identified, including E coli, Enterococcus faecalis, and Bacteroides fragilis. Unfortunately, there are also bacteria such as Fusobacterium species and Streptococcus gallolyticus with the potential to alter intestinal permeability, resulting in downstream effects that can allow colon cancers to expand. Fusobacterium species and Streptococcus gallolyticus have the potential to cause DNA double–strand breaks in the intestine, which can produce chromosomal precariousness.
These secondary bacteria can also lead to DNA epigenetic changes and gene mutations. However, it should be emphasized that “the direct causation of imprinted DNA changes resulting from a direct interaction between bacteria and host cells is not so far established.”
E coli produces compounds called cyclomodulins, which can cause DNA breaks and potentially trigger cell cycle arrest and even cell death through activation of the DNA damage checkpoint pathway. The DNA damage checkpoint pathway is a cellular signaling network that helps detect DNA lesions and allows for genetic stability by stopping growth to allow for repair and simulating cell survival or apoptosis. A key cyclomodulin that E coli makes is colibactin, produced by the pks locus. Other cyclomodulins include cytolethal distending toxin, cytotoxic necrotizing factor, and cycle-inhibiting factor.
Previous research has shown that E coli is the only culturable bacteria found near CRC. A groundbreaking 1998 study employing PCR technology found E coli in 60% of colon polyp adenomas and an alarming 77% of CRC biopsies.
E coli’s capability to downregulate essential DNA mismatch repair proteins has been implicated in colorectal carcinogenesis. Interestingly, when the genetic region responsible for producing colibactin is deleted in animals, the bacteria aren’t able to promote cancer.
Mechanistically, colibactin causes double-stranded DNA breaks, eukaryotic cell cycle arrest, and chromosome abnormalities. It also alkylates DNA. This occurs when the cyclopropane ring of colibactin interacts with the N3 position of adenine in DNA, forming a covalent bond and creating a DNA adduct. DNA adducts occur when a chemical moiety from an environmental or dietary source binds to DNA base. Colibactin can cause DNA interstrand cross-links to form via alkalization of adenine residues on opposing DNA strands, a crucial step in DNA damage. DNA adducts can occur through carcinogens in N-nitroso compounds, such as in processed meats and in polycyclic aromatic hydrocarbons found in cigarette smoke. Colibactin-induced damage may also stimulate the senescence–associated secretory phenotype pathway, increasing proinflammatory cytokines.
E coli and Inflammatory Bowel Disease
E coli, the primary colibactin producer in the human intestinal microbiome, is found at higher bacterial percentages in the microbiomes of patients with inflammatory bowel disease (IBD). In a study by Dubinsky and colleagues, “the medium relative levels of colibactin–encoding E. coli were about threefold higher in IBD.”
Researchers have also postulated that antibiotics and microbiome dysbiosis may create conditions that allow colibactin–producing bacteria to overpopulate.
Future Directions
Not every patient with CRC carries a colorectal mutational signature, but these findings underscore the need for continued vigilance and prevention.
From a public health standpoint, our advice remains consistent: Promote high-fiber diets with more vegetables and less red meat; avoid highly processed foods; avoid alcohol; encourage exercise; and address overweight and obesity. Our goal is to create the best possible colon environment to prevent DNA damage from bacterial and environmental carcinogens.
In the future, we need more research to clarify exactly how E coli and colibactin increase early–onset CRC risk and whether antibiotics and dysbiosis facilitate their ability to damage the DNA of colon mucosa. It’s still unclear why younger patients are at greater risk. In time, we may be able to screen for colibactin–producing bacteria such as E coli and manipulate the fecal microbiome to prevent damage.
A recent mouse study in Nature by Jans and colleagues suggests it might be possible to block bacterial adhesion and hopefully mitigate damage caused by colibactin. With continued work, colibactin–targeted strategies could become a part of CRC prevention.
Benjamin H. Levy III, MD, is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who gave a TEDx Talk about building health education campaigns using music and concerts, organizes "Tune It Up: A Concert To Raise Colorectal Cancer Awareness" with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee.
A version of this article first appeared on Medscape.com.
Is There Really a Cancer Epidemic in Younger Adults?
A global analysis challenged the notion that a rise in cancer is disproportionately affecting younger adults, finding instead that several cancer types previously seen rising in younger adults are also increasing in older adults.
More specifically, the analysis found that incidence rates for thyroid cancer, breast cancer, kidney cancer, endometrial cancer, and leukemia increased similarly in both younger and older adults in most countries over a 15-year period. Colorectal cancer (CRC) was the exception, where incidence rates increased in younger adults in most countries but only increased slightly in older adults in about half and decreased in about one quarter.
“Our findings suggest that whatever is triggering the rise in these cancers is more likely to be common across all age groups, rather than specific to cancers in the under 50s, since there were similar increases in younger and older adults,” Amy Berrington de González, DPhil, The Institute of Cancer Research, London, England, who led the study, said in a statement.
The authors of an editorial agreed, adding that the growing “concern about increasing cancer rates should recognize that this increase is not restricted to young adults but affects all generations.”
The study and editorial were published recently in Annals of Internal Medicine.
Data Defy Early-Onset Cancer Epidemic Narrative
A growing body of evidence suggests that cancer incidence rates are increasing among younger adults in many countries. However, studies tracking international trends have largely evaluated cancer incidence in younger adults without comparing these trends in older adults or analyses have focused the age comparison in individual countries, Berrington de González and colleagues explained.
To better understand cancer incidence trends across countries and age groups, the researchers evaluated cancer trends in 42 countries between 2003 and 2017, focusing on 13 cancer types previously reported to be climbing in adults younger than age 50 years.
The researchers found that incidence rates for six of the 13 cancer types increased among younger adults (aged 20-49 years) in more than three quarters of the countries studied.
The largest increase was in thyroid cancer (median average annual percentage change [AAPC], 3.57%), followed by kidney cancer (median AAPC, 2.21%), endometrial cancer (median AAPC, 1.66%), CRC (median AAPC, 1.45%), breast cancer (median AAPC, 0.89%), and leukemia (median AAPC, 0.78%).
But with the exception of CRC, incidence rates for these cancers increased to a similar degree in adults aged 50 years or older — with median AAPCs of 3% (vs 3.57%) for thyroid cancer, 1.65% (vs 2.21%) for kidney cancer, 1.20% (vs 1.66%) for endometrial cancer, 0.86% (vs 0.89%) for breast cancer, and 0.61% (vs 0.78%) for leukemia.
In older adults, CRC incidence rates only increased in about half the countries (median AAPC, 0.37%), and the annual percentage change was much greater in younger than older adults in nearly 70% of countries. CRC incidence rates in older individuals also decreased in nearly 25% of countries.
Why is CRC an apparent outlier?
“Bowel cancer screening not only helps detect cancer at earlier stages but also helps prevent cancer through the removal of premalignant lesions,” Berrington de González said. “This could be why bowel cancer cases seem to be rising faster in younger adults — we’re getting better at preventing them developing in older adults.”
The incidence of certain cancers also declined in younger adults. Specifically, rates of liver, oral, esophageal, and stomach cancers decreased in younger adults in more than half of countries assessed, with median AAPCs of -0.14% for liver, -0.42% for oral, -0.92% for esophageal, and -1.62% for stomach cancers.
Over half of countries also saw declining rates of stomach (median AAPC, -2.05%) and esophageal (median AAPC, -0.25%) cancers among older adults, while rates of liver and oral cancers increased in older individuals (median AAPC, 2.17% and 0.49%, respectively).
For gallbladder, pancreatic, and prostate cancers — three other cancers previously found to be increasing in younger adults — the researchers reported that incidence rates increased in younger adults in just over half of countries (median AAPCs, 3.2% for prostate cancer, 0.49% for gallbladder cancer, and 1% for pancreatic cancer). Incidence rates also often increased in older adults but to a lesser extent (median AAPCs, 0.75% for prostate cancer, -0.10% for gallbladder, and 0.96% for pancreatic cancer).
True Rise or Increased Scrutiny?
Why are cancer rates increasing?
“Understanding factors that contribute to the increase in incidence across the age spectrum was beyond the scope of the study,” editorialists Christopher Cann, MD, Fox Chase Cancer Center, and Efrat Dotan, MD, University of Pennsylvania Health System, both in Philadelphia, wrote.
Several studies have suggested that rising rates of obesity could help explain increasing cancer incidence, particularly in younger adults. In fact, “the cancers that we identified as increasing are all obesity-related cancers, including endometrial and kidney cancer,” Berrington de González said. However, so far, the evidence on this link remains unclear, she acknowledged.
Weighing in on the study, Gilbert Welch, MD, Brigham and Women’s Hospital, Boston, told this news organization that it’s “critically important” to distinguish between two explanations for rising cancer incidence.
There may be an increase in the true occurrence of clinically meaningful cancer, which “warrants investigation into biologic explanations, better treatment, and perhaps more testing,” Welch said.
But it may instead reflect changes in diagnostic scrutiny. “Simply put, whenever we doctors look harder for cancer, we find more,” Welch said. “And there are lots of ways to look harder: testing more people, testing people more frequently, using tests with increasing ability to detect small irregularities, and using lower diagnostic thresholds for labeling these as cancer.”
If increased incidence is the result of greater diagnostic scrutiny, searching for biologic causes is bound to be unproductive and more testing will only aggravate the problem, he explained.
Welch pointed out that the fastest rising cancer in both younger and older adults was thyroid cancer (AAPC, ≥ 3%), which is “exquisitely sensitive” to diagnostic scrutiny.
Take what happened in South Korea. Around 2000, the government of South Korea started a national screening program for breast, colon, and stomach cancers. Doctors and hospitals often added on ultrasound scans for thyroid cancer for a small additional fee.
“A decade later the rate of thyroid cancer diagnosis had increased 15-fold, turning what was once a rare cancer into the most common cancer in Korea,” Welch said. “But the death rate from thyroid cancer did not change. This was not an epidemic of disease; this was an epidemic of diagnosis.”
Welch also noted that the study authors and editorialists put the finding in perspective by explaining that, despite the rising rates of certain cancers in younger adults, cancer remains rare in these adults.
Welch highlighted that, for younger adults in the US, cancer death rates in young adults have cut in half over the last 30 years. “Cancer accounts for only 10% of deaths in young people in the US — and that number is falling,” Welch said.
The study was funded by the Institute of Cancer Research and the National Institutes of Health Intramural Research Program. Disclosures for authors and editorial writers are available with the original articles. Welch reported receiving royalties from three books including “Should I be tested for cancer?”
A version of this article first appeared on Medscape.com.
A global analysis challenged the notion that a rise in cancer is disproportionately affecting younger adults, finding instead that several cancer types previously seen rising in younger adults are also increasing in older adults.
More specifically, the analysis found that incidence rates for thyroid cancer, breast cancer, kidney cancer, endometrial cancer, and leukemia increased similarly in both younger and older adults in most countries over a 15-year period. Colorectal cancer (CRC) was the exception, where incidence rates increased in younger adults in most countries but only increased slightly in older adults in about half and decreased in about one quarter.
“Our findings suggest that whatever is triggering the rise in these cancers is more likely to be common across all age groups, rather than specific to cancers in the under 50s, since there were similar increases in younger and older adults,” Amy Berrington de González, DPhil, The Institute of Cancer Research, London, England, who led the study, said in a statement.
The authors of an editorial agreed, adding that the growing “concern about increasing cancer rates should recognize that this increase is not restricted to young adults but affects all generations.”
The study and editorial were published recently in Annals of Internal Medicine.
Data Defy Early-Onset Cancer Epidemic Narrative
A growing body of evidence suggests that cancer incidence rates are increasing among younger adults in many countries. However, studies tracking international trends have largely evaluated cancer incidence in younger adults without comparing these trends in older adults or analyses have focused the age comparison in individual countries, Berrington de González and colleagues explained.
To better understand cancer incidence trends across countries and age groups, the researchers evaluated cancer trends in 42 countries between 2003 and 2017, focusing on 13 cancer types previously reported to be climbing in adults younger than age 50 years.
The researchers found that incidence rates for six of the 13 cancer types increased among younger adults (aged 20-49 years) in more than three quarters of the countries studied.
The largest increase was in thyroid cancer (median average annual percentage change [AAPC], 3.57%), followed by kidney cancer (median AAPC, 2.21%), endometrial cancer (median AAPC, 1.66%), CRC (median AAPC, 1.45%), breast cancer (median AAPC, 0.89%), and leukemia (median AAPC, 0.78%).
But with the exception of CRC, incidence rates for these cancers increased to a similar degree in adults aged 50 years or older — with median AAPCs of 3% (vs 3.57%) for thyroid cancer, 1.65% (vs 2.21%) for kidney cancer, 1.20% (vs 1.66%) for endometrial cancer, 0.86% (vs 0.89%) for breast cancer, and 0.61% (vs 0.78%) for leukemia.
In older adults, CRC incidence rates only increased in about half the countries (median AAPC, 0.37%), and the annual percentage change was much greater in younger than older adults in nearly 70% of countries. CRC incidence rates in older individuals also decreased in nearly 25% of countries.
Why is CRC an apparent outlier?
“Bowel cancer screening not only helps detect cancer at earlier stages but also helps prevent cancer through the removal of premalignant lesions,” Berrington de González said. “This could be why bowel cancer cases seem to be rising faster in younger adults — we’re getting better at preventing them developing in older adults.”
The incidence of certain cancers also declined in younger adults. Specifically, rates of liver, oral, esophageal, and stomach cancers decreased in younger adults in more than half of countries assessed, with median AAPCs of -0.14% for liver, -0.42% for oral, -0.92% for esophageal, and -1.62% for stomach cancers.
Over half of countries also saw declining rates of stomach (median AAPC, -2.05%) and esophageal (median AAPC, -0.25%) cancers among older adults, while rates of liver and oral cancers increased in older individuals (median AAPC, 2.17% and 0.49%, respectively).
For gallbladder, pancreatic, and prostate cancers — three other cancers previously found to be increasing in younger adults — the researchers reported that incidence rates increased in younger adults in just over half of countries (median AAPCs, 3.2% for prostate cancer, 0.49% for gallbladder cancer, and 1% for pancreatic cancer). Incidence rates also often increased in older adults but to a lesser extent (median AAPCs, 0.75% for prostate cancer, -0.10% for gallbladder, and 0.96% for pancreatic cancer).
True Rise or Increased Scrutiny?
Why are cancer rates increasing?
“Understanding factors that contribute to the increase in incidence across the age spectrum was beyond the scope of the study,” editorialists Christopher Cann, MD, Fox Chase Cancer Center, and Efrat Dotan, MD, University of Pennsylvania Health System, both in Philadelphia, wrote.
Several studies have suggested that rising rates of obesity could help explain increasing cancer incidence, particularly in younger adults. In fact, “the cancers that we identified as increasing are all obesity-related cancers, including endometrial and kidney cancer,” Berrington de González said. However, so far, the evidence on this link remains unclear, she acknowledged.
Weighing in on the study, Gilbert Welch, MD, Brigham and Women’s Hospital, Boston, told this news organization that it’s “critically important” to distinguish between two explanations for rising cancer incidence.
There may be an increase in the true occurrence of clinically meaningful cancer, which “warrants investigation into biologic explanations, better treatment, and perhaps more testing,” Welch said.
But it may instead reflect changes in diagnostic scrutiny. “Simply put, whenever we doctors look harder for cancer, we find more,” Welch said. “And there are lots of ways to look harder: testing more people, testing people more frequently, using tests with increasing ability to detect small irregularities, and using lower diagnostic thresholds for labeling these as cancer.”
If increased incidence is the result of greater diagnostic scrutiny, searching for biologic causes is bound to be unproductive and more testing will only aggravate the problem, he explained.
Welch pointed out that the fastest rising cancer in both younger and older adults was thyroid cancer (AAPC, ≥ 3%), which is “exquisitely sensitive” to diagnostic scrutiny.
Take what happened in South Korea. Around 2000, the government of South Korea started a national screening program for breast, colon, and stomach cancers. Doctors and hospitals often added on ultrasound scans for thyroid cancer for a small additional fee.
“A decade later the rate of thyroid cancer diagnosis had increased 15-fold, turning what was once a rare cancer into the most common cancer in Korea,” Welch said. “But the death rate from thyroid cancer did not change. This was not an epidemic of disease; this was an epidemic of diagnosis.”
Welch also noted that the study authors and editorialists put the finding in perspective by explaining that, despite the rising rates of certain cancers in younger adults, cancer remains rare in these adults.
Welch highlighted that, for younger adults in the US, cancer death rates in young adults have cut in half over the last 30 years. “Cancer accounts for only 10% of deaths in young people in the US — and that number is falling,” Welch said.
The study was funded by the Institute of Cancer Research and the National Institutes of Health Intramural Research Program. Disclosures for authors and editorial writers are available with the original articles. Welch reported receiving royalties from three books including “Should I be tested for cancer?”
A version of this article first appeared on Medscape.com.
A global analysis challenged the notion that a rise in cancer is disproportionately affecting younger adults, finding instead that several cancer types previously seen rising in younger adults are also increasing in older adults.
More specifically, the analysis found that incidence rates for thyroid cancer, breast cancer, kidney cancer, endometrial cancer, and leukemia increased similarly in both younger and older adults in most countries over a 15-year period. Colorectal cancer (CRC) was the exception, where incidence rates increased in younger adults in most countries but only increased slightly in older adults in about half and decreased in about one quarter.
“Our findings suggest that whatever is triggering the rise in these cancers is more likely to be common across all age groups, rather than specific to cancers in the under 50s, since there were similar increases in younger and older adults,” Amy Berrington de González, DPhil, The Institute of Cancer Research, London, England, who led the study, said in a statement.
The authors of an editorial agreed, adding that the growing “concern about increasing cancer rates should recognize that this increase is not restricted to young adults but affects all generations.”
The study and editorial were published recently in Annals of Internal Medicine.
Data Defy Early-Onset Cancer Epidemic Narrative
A growing body of evidence suggests that cancer incidence rates are increasing among younger adults in many countries. However, studies tracking international trends have largely evaluated cancer incidence in younger adults without comparing these trends in older adults or analyses have focused the age comparison in individual countries, Berrington de González and colleagues explained.
To better understand cancer incidence trends across countries and age groups, the researchers evaluated cancer trends in 42 countries between 2003 and 2017, focusing on 13 cancer types previously reported to be climbing in adults younger than age 50 years.
The researchers found that incidence rates for six of the 13 cancer types increased among younger adults (aged 20-49 years) in more than three quarters of the countries studied.
The largest increase was in thyroid cancer (median average annual percentage change [AAPC], 3.57%), followed by kidney cancer (median AAPC, 2.21%), endometrial cancer (median AAPC, 1.66%), CRC (median AAPC, 1.45%), breast cancer (median AAPC, 0.89%), and leukemia (median AAPC, 0.78%).
But with the exception of CRC, incidence rates for these cancers increased to a similar degree in adults aged 50 years or older — with median AAPCs of 3% (vs 3.57%) for thyroid cancer, 1.65% (vs 2.21%) for kidney cancer, 1.20% (vs 1.66%) for endometrial cancer, 0.86% (vs 0.89%) for breast cancer, and 0.61% (vs 0.78%) for leukemia.
In older adults, CRC incidence rates only increased in about half the countries (median AAPC, 0.37%), and the annual percentage change was much greater in younger than older adults in nearly 70% of countries. CRC incidence rates in older individuals also decreased in nearly 25% of countries.
Why is CRC an apparent outlier?
“Bowel cancer screening not only helps detect cancer at earlier stages but also helps prevent cancer through the removal of premalignant lesions,” Berrington de González said. “This could be why bowel cancer cases seem to be rising faster in younger adults — we’re getting better at preventing them developing in older adults.”
The incidence of certain cancers also declined in younger adults. Specifically, rates of liver, oral, esophageal, and stomach cancers decreased in younger adults in more than half of countries assessed, with median AAPCs of -0.14% for liver, -0.42% for oral, -0.92% for esophageal, and -1.62% for stomach cancers.
Over half of countries also saw declining rates of stomach (median AAPC, -2.05%) and esophageal (median AAPC, -0.25%) cancers among older adults, while rates of liver and oral cancers increased in older individuals (median AAPC, 2.17% and 0.49%, respectively).
For gallbladder, pancreatic, and prostate cancers — three other cancers previously found to be increasing in younger adults — the researchers reported that incidence rates increased in younger adults in just over half of countries (median AAPCs, 3.2% for prostate cancer, 0.49% for gallbladder cancer, and 1% for pancreatic cancer). Incidence rates also often increased in older adults but to a lesser extent (median AAPCs, 0.75% for prostate cancer, -0.10% for gallbladder, and 0.96% for pancreatic cancer).
True Rise or Increased Scrutiny?
Why are cancer rates increasing?
“Understanding factors that contribute to the increase in incidence across the age spectrum was beyond the scope of the study,” editorialists Christopher Cann, MD, Fox Chase Cancer Center, and Efrat Dotan, MD, University of Pennsylvania Health System, both in Philadelphia, wrote.
Several studies have suggested that rising rates of obesity could help explain increasing cancer incidence, particularly in younger adults. In fact, “the cancers that we identified as increasing are all obesity-related cancers, including endometrial and kidney cancer,” Berrington de González said. However, so far, the evidence on this link remains unclear, she acknowledged.
Weighing in on the study, Gilbert Welch, MD, Brigham and Women’s Hospital, Boston, told this news organization that it’s “critically important” to distinguish between two explanations for rising cancer incidence.
There may be an increase in the true occurrence of clinically meaningful cancer, which “warrants investigation into biologic explanations, better treatment, and perhaps more testing,” Welch said.
But it may instead reflect changes in diagnostic scrutiny. “Simply put, whenever we doctors look harder for cancer, we find more,” Welch said. “And there are lots of ways to look harder: testing more people, testing people more frequently, using tests with increasing ability to detect small irregularities, and using lower diagnostic thresholds for labeling these as cancer.”
If increased incidence is the result of greater diagnostic scrutiny, searching for biologic causes is bound to be unproductive and more testing will only aggravate the problem, he explained.
Welch pointed out that the fastest rising cancer in both younger and older adults was thyroid cancer (AAPC, ≥ 3%), which is “exquisitely sensitive” to diagnostic scrutiny.
Take what happened in South Korea. Around 2000, the government of South Korea started a national screening program for breast, colon, and stomach cancers. Doctors and hospitals often added on ultrasound scans for thyroid cancer for a small additional fee.
“A decade later the rate of thyroid cancer diagnosis had increased 15-fold, turning what was once a rare cancer into the most common cancer in Korea,” Welch said. “But the death rate from thyroid cancer did not change. This was not an epidemic of disease; this was an epidemic of diagnosis.”
Welch also noted that the study authors and editorialists put the finding in perspective by explaining that, despite the rising rates of certain cancers in younger adults, cancer remains rare in these adults.
Welch highlighted that, for younger adults in the US, cancer death rates in young adults have cut in half over the last 30 years. “Cancer accounts for only 10% of deaths in young people in the US — and that number is falling,” Welch said.
The study was funded by the Institute of Cancer Research and the National Institutes of Health Intramural Research Program. Disclosures for authors and editorial writers are available with the original articles. Welch reported receiving royalties from three books including “Should I be tested for cancer?”
A version of this article first appeared on Medscape.com.
LLMs Show High Accuracy in Extracting CRC Data From VA Health Records
TOPLINE: Large Language Models (LLMs) achieve more than 95% accuracy in extracting colorectal cancer and dysplasia diagnoses from Veterans Health Administration (VHA) pathology reports, including patients with Million Veteran Program (MVP) genomic data. The validated approach using publicly available LLMs demonstrates excellent performance across both Inflammatory Bowel Disease (IBD) and non-IBD populations.
METHODOLOGY:
Researchers analyzed 116,373 pathology reports generated in the VHA between 1999 and 2024, utilizing search term filtering followed by simple yes/no question prompts for identifying colorectal dysplasia, high-grade dysplasia and/or colorectal adenocarcinoma, and invasive colorectal cancer.
Results were compared to blinded manual chart review of 200 to 300 pathology reports for each patient cohort and diagnostic task, totaling 3,816 reviewed reports, to validate the LLM approach.
Validation was performed independently in IBD and non-IBD populations using Gemma-2 and Llama-3 LLMs without any task-specific training or fine-tuning.
Performance metrics included F1 scores, positive predictive value, negative predictive value, sensitivity, specificity, and Matthew's correlation coefficient to evaluate accuracy across different tasks.
TAKEAWAY:
In patients with IBD in the MVP, the LLM achieved (F1-score, 96.9%; 95% confidence interval [CI], 94.0%-99.6%) for identifying dysplasia, (F1-score, 93.7%; 95% CI, 88.2%-98.4%) for identifying high-grade dysplasia/colorectal cancer, and (F1-score, 98%; 95% CI, 96.3%-99.4%) for identifying colorectal cancer.
In non-IBD MVP patients, the LLM demonstrated (F1-score, 99.2%; 95% CI, 98.2%-100%) for identifying colorectal dysplasia, (F1-score, 96.5%; 95% CI, 93.0%-99.2%) for high-grade dysplasia/colorectal cancer, and (F1-score, 95%; 95% CI, 92.8%-97.2%) for identifying colorectal cancer.
Agreement between reviewers was excellent across tasks, with (Cohen's kappa, 89%-97%) for main tasks, and (Cohen's kappa, 78.1%-93.1%) for indefinite for dysplasia in IBD cohort.
The LLM approach maintained high accuracy when applied to full pathology reports, with (F1-score, 97.1%; 95% CI, 93.5%-100%) for dysplasia detection in IBD patients.
IN PRACTICE: “We have shown that LLMs are powerful, potentially generalizable tools for accurately extracting important information from clinical semistructured and unstructured text and which require little human-led development.” the authors of the study wrote
SOURCE: The study was based on data from the Million Veteran Program and supported by the Office of Research and Development, Veterans Health Administration, and the US Department of Veterans Affairs Biomedical Laboratory. It was published online in BMJ Open Gastroenterology.
LIMITATIONS: According to the authors, this research may be specific to the VHA system and the LLM models used. The authors did not test larger models. The authors acknowledge that without long-term access to graphics processing units, they could not feasibly test larger models, which may overcome some of the shortcomings seen in smaller models. Additionally, the researchers could not rule out overlap between Million Veteran Program and Corporate Data Warehouse reports, though they state that results in either cohort alone are sufficient validation compared with previously published work.
DISCLOSURES: The study was supported by Merit Review Award from the United States Department of Veterans Affairs Biomedical Laboratory Research and Development Service, AGA Research Foundation, National Institutes of Health grants, and the National Library of Medicine Training Grant. Kit Curtius reported receiving an investigator-led research grant from Phathom Pharmaceuticals. Shailja C Shah disclosed being a paid consultant for RedHill Biopharma and Phathom Pharmaceuticals, and an unpaid scientific advisory board member for Ilico Genetics, Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: Large Language Models (LLMs) achieve more than 95% accuracy in extracting colorectal cancer and dysplasia diagnoses from Veterans Health Administration (VHA) pathology reports, including patients with Million Veteran Program (MVP) genomic data. The validated approach using publicly available LLMs demonstrates excellent performance across both Inflammatory Bowel Disease (IBD) and non-IBD populations.
METHODOLOGY:
Researchers analyzed 116,373 pathology reports generated in the VHA between 1999 and 2024, utilizing search term filtering followed by simple yes/no question prompts for identifying colorectal dysplasia, high-grade dysplasia and/or colorectal adenocarcinoma, and invasive colorectal cancer.
Results were compared to blinded manual chart review of 200 to 300 pathology reports for each patient cohort and diagnostic task, totaling 3,816 reviewed reports, to validate the LLM approach.
Validation was performed independently in IBD and non-IBD populations using Gemma-2 and Llama-3 LLMs without any task-specific training or fine-tuning.
Performance metrics included F1 scores, positive predictive value, negative predictive value, sensitivity, specificity, and Matthew's correlation coefficient to evaluate accuracy across different tasks.
TAKEAWAY:
In patients with IBD in the MVP, the LLM achieved (F1-score, 96.9%; 95% confidence interval [CI], 94.0%-99.6%) for identifying dysplasia, (F1-score, 93.7%; 95% CI, 88.2%-98.4%) for identifying high-grade dysplasia/colorectal cancer, and (F1-score, 98%; 95% CI, 96.3%-99.4%) for identifying colorectal cancer.
In non-IBD MVP patients, the LLM demonstrated (F1-score, 99.2%; 95% CI, 98.2%-100%) for identifying colorectal dysplasia, (F1-score, 96.5%; 95% CI, 93.0%-99.2%) for high-grade dysplasia/colorectal cancer, and (F1-score, 95%; 95% CI, 92.8%-97.2%) for identifying colorectal cancer.
Agreement between reviewers was excellent across tasks, with (Cohen's kappa, 89%-97%) for main tasks, and (Cohen's kappa, 78.1%-93.1%) for indefinite for dysplasia in IBD cohort.
The LLM approach maintained high accuracy when applied to full pathology reports, with (F1-score, 97.1%; 95% CI, 93.5%-100%) for dysplasia detection in IBD patients.
IN PRACTICE: “We have shown that LLMs are powerful, potentially generalizable tools for accurately extracting important information from clinical semistructured and unstructured text and which require little human-led development.” the authors of the study wrote
SOURCE: The study was based on data from the Million Veteran Program and supported by the Office of Research and Development, Veterans Health Administration, and the US Department of Veterans Affairs Biomedical Laboratory. It was published online in BMJ Open Gastroenterology.
LIMITATIONS: According to the authors, this research may be specific to the VHA system and the LLM models used. The authors did not test larger models. The authors acknowledge that without long-term access to graphics processing units, they could not feasibly test larger models, which may overcome some of the shortcomings seen in smaller models. Additionally, the researchers could not rule out overlap between Million Veteran Program and Corporate Data Warehouse reports, though they state that results in either cohort alone are sufficient validation compared with previously published work.
DISCLOSURES: The study was supported by Merit Review Award from the United States Department of Veterans Affairs Biomedical Laboratory Research and Development Service, AGA Research Foundation, National Institutes of Health grants, and the National Library of Medicine Training Grant. Kit Curtius reported receiving an investigator-led research grant from Phathom Pharmaceuticals. Shailja C Shah disclosed being a paid consultant for RedHill Biopharma and Phathom Pharmaceuticals, and an unpaid scientific advisory board member for Ilico Genetics, Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: Large Language Models (LLMs) achieve more than 95% accuracy in extracting colorectal cancer and dysplasia diagnoses from Veterans Health Administration (VHA) pathology reports, including patients with Million Veteran Program (MVP) genomic data. The validated approach using publicly available LLMs demonstrates excellent performance across both Inflammatory Bowel Disease (IBD) and non-IBD populations.
METHODOLOGY:
Researchers analyzed 116,373 pathology reports generated in the VHA between 1999 and 2024, utilizing search term filtering followed by simple yes/no question prompts for identifying colorectal dysplasia, high-grade dysplasia and/or colorectal adenocarcinoma, and invasive colorectal cancer.
Results were compared to blinded manual chart review of 200 to 300 pathology reports for each patient cohort and diagnostic task, totaling 3,816 reviewed reports, to validate the LLM approach.
Validation was performed independently in IBD and non-IBD populations using Gemma-2 and Llama-3 LLMs without any task-specific training or fine-tuning.
Performance metrics included F1 scores, positive predictive value, negative predictive value, sensitivity, specificity, and Matthew's correlation coefficient to evaluate accuracy across different tasks.
TAKEAWAY:
In patients with IBD in the MVP, the LLM achieved (F1-score, 96.9%; 95% confidence interval [CI], 94.0%-99.6%) for identifying dysplasia, (F1-score, 93.7%; 95% CI, 88.2%-98.4%) for identifying high-grade dysplasia/colorectal cancer, and (F1-score, 98%; 95% CI, 96.3%-99.4%) for identifying colorectal cancer.
In non-IBD MVP patients, the LLM demonstrated (F1-score, 99.2%; 95% CI, 98.2%-100%) for identifying colorectal dysplasia, (F1-score, 96.5%; 95% CI, 93.0%-99.2%) for high-grade dysplasia/colorectal cancer, and (F1-score, 95%; 95% CI, 92.8%-97.2%) for identifying colorectal cancer.
Agreement between reviewers was excellent across tasks, with (Cohen's kappa, 89%-97%) for main tasks, and (Cohen's kappa, 78.1%-93.1%) for indefinite for dysplasia in IBD cohort.
The LLM approach maintained high accuracy when applied to full pathology reports, with (F1-score, 97.1%; 95% CI, 93.5%-100%) for dysplasia detection in IBD patients.
IN PRACTICE: “We have shown that LLMs are powerful, potentially generalizable tools for accurately extracting important information from clinical semistructured and unstructured text and which require little human-led development.” the authors of the study wrote
SOURCE: The study was based on data from the Million Veteran Program and supported by the Office of Research and Development, Veterans Health Administration, and the US Department of Veterans Affairs Biomedical Laboratory. It was published online in BMJ Open Gastroenterology.
LIMITATIONS: According to the authors, this research may be specific to the VHA system and the LLM models used. The authors did not test larger models. The authors acknowledge that without long-term access to graphics processing units, they could not feasibly test larger models, which may overcome some of the shortcomings seen in smaller models. Additionally, the researchers could not rule out overlap between Million Veteran Program and Corporate Data Warehouse reports, though they state that results in either cohort alone are sufficient validation compared with previously published work.
DISCLOSURES: The study was supported by Merit Review Award from the United States Department of Veterans Affairs Biomedical Laboratory Research and Development Service, AGA Research Foundation, National Institutes of Health grants, and the National Library of Medicine Training Grant. Kit Curtius reported receiving an investigator-led research grant from Phathom Pharmaceuticals. Shailja C Shah disclosed being a paid consultant for RedHill Biopharma and Phathom Pharmaceuticals, and an unpaid scientific advisory board member for Ilico Genetics, Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Patients With a Positive FIT Fail to Get Follow-Up Colonoscopies
Patients With a Positive FIT Fail to Get Follow-Up Colonoscopies
PHOENIX -- Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
"In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy," said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings this week at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
"These findings reinforce the importance of colonoscopy following positive interval FIT, given the high risk of advanced neoplasia and colorectal cancer, regardless of polypectomy history," Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, due to the higher risk.
Reasons patients may instead turn to FIT include cost or other factors.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2004.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the nonpolypectomy group).
Among the FIT screenings, results were positive in 17.2% of postpolypectomy patients and 14.1% of patients who no prior polypectomy, indicating a history of polypectomy to be predictive of positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result -- and having a previous polypectomy should add further emergency to the matter -- the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the nonpolypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the postcolonoscopy interval FIT.
The findings underscore that "positive results carried a high risk of advanced neoplasia or cancer, irrespective or prior polypectomy history," Wilson said.
Commenting on the study, William D. Chey, MD, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, Michigan, noted that the study "addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy."
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
"Other data suggest that the rate might even be significantly higher -- at 70% to 80%, depending upon the population and the test," Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies "should raise questions about whether there might be a role for FIT testing in addition to colonoscopy." However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is "how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy," he said.
"I think a lot of this is going to come down to how it's down at the primary care level."
Chey added that in that, and any other setting, "the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it's positive, a follow-up colonoscopy must be performed.
"Otherwise, the stool-based test is of no value."
Wilson had no disclosures to report. Chey's disclosures include consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestle, Phathom, Redhill, Salix/Valean, Takeda, and Vibrant.
A version of this article first appeared on Medscape.com.
PHOENIX -- Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
"In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy," said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings this week at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
"These findings reinforce the importance of colonoscopy following positive interval FIT, given the high risk of advanced neoplasia and colorectal cancer, regardless of polypectomy history," Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, due to the higher risk.
Reasons patients may instead turn to FIT include cost or other factors.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2004.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the nonpolypectomy group).
Among the FIT screenings, results were positive in 17.2% of postpolypectomy patients and 14.1% of patients who no prior polypectomy, indicating a history of polypectomy to be predictive of positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result -- and having a previous polypectomy should add further emergency to the matter -- the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the nonpolypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the postcolonoscopy interval FIT.
The findings underscore that "positive results carried a high risk of advanced neoplasia or cancer, irrespective or prior polypectomy history," Wilson said.
Commenting on the study, William D. Chey, MD, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, Michigan, noted that the study "addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy."
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
"Other data suggest that the rate might even be significantly higher -- at 70% to 80%, depending upon the population and the test," Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies "should raise questions about whether there might be a role for FIT testing in addition to colonoscopy." However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is "how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy," he said.
"I think a lot of this is going to come down to how it's down at the primary care level."
Chey added that in that, and any other setting, "the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it's positive, a follow-up colonoscopy must be performed.
"Otherwise, the stool-based test is of no value."
Wilson had no disclosures to report. Chey's disclosures include consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestle, Phathom, Redhill, Salix/Valean, Takeda, and Vibrant.
A version of this article first appeared on Medscape.com.
PHOENIX -- Patients with or without polyp removal in an index colonoscopy commonly receive follow-up surveillance with a fecal immunochemical test (FIT), yet many of these patients do not receive a recommended colonoscopy after a positive FIT.
"In this large US study, we found interval FITs are frequently performed in patients with and without prior polypectomy," said first author Natalie J. Wilson, MD, of the University of Minnesota in Minneapolis, while presenting the findings this week at the American College of Gastroenterology (ACG) 2025 Annual Scientific Meeting.
"These findings reinforce the importance of colonoscopy following positive interval FIT, given the high risk of advanced neoplasia and colorectal cancer, regardless of polypectomy history," Wilson said.
Guideline recommendations stress the need for follow-up surveillance with a colonoscopy, particularly in patients who have had a prior polypectomy, due to the higher risk.
Reasons patients may instead turn to FIT include cost or other factors.
To determine just how often that happens, how having a previous polypectomy affects FIT results, and how adherent patients are to follow up if a FIT result is positive, Wilson and her colleagues evaluated data from nearly 4.8 million individuals in the Veterans Health Administration Corporate Data Warehouse who underwent colonoscopy between 2000 and 2004.
Of the patients, 10.9% were found to have subsequently received interval FIT within 10 years of the index colonoscopy, and of those patients, nearly half (49.9%) had received a polypectomy at the index colonoscopy.
The average time from the colonoscopy/polypectomy to the interval FIT was 5.9 years (5.6 years in the polypectomy group vs 6.2 years in the nonpolypectomy group).
Among the FIT screenings, results were positive in 17.2% of postpolypectomy patients and 14.1% of patients who no prior polypectomy, indicating a history of polypectomy to be predictive of positive interval FIT (odds ratio [OR], 1.12; P < .0001).
Notably, while a follow-up colonoscopy is considered essential following a positive FIT result -- and having a previous polypectomy should add further emergency to the matter -- the study showed only 50.4% of those who had an earlier polypectomy went on to receive the recommended follow-up colonoscopy after a positive follow-up FIT, and the rate was 49.3% among those who had not received a polypectomy (P = .001).
For those who did receive a follow-up colonoscopy after a positive FIT, the duration of time to receiving the colonoscopy was longer among those who had a prior polypectomy, at 2.9 months compared with 2.5 months in the nonpolypectomy group (P < .001).
Colonoscopy results following a positive FIT showed higher rates of detections among patients who had prior polypectomies than among those with no prior polypectomy, including tubular adenomas (54.7% vs 45.8%), tubulovillous adenomas (5.6% vs 4.7%), adenomas with high-grade dysplasia (0.8% vs 0.7%), sessile serrated lesions (3.52% vs 2.4%), advanced colorectal neoplasia (9.2% vs 7.9%), and colorectal cancer (3.3% vs 3.0%).
However, a prior polypectomy was not independently predictive of colorectal cancer (OR, 0.96; P = .65) or advanced colorectal neoplasia (OR, 0.97; P = .57) in the postcolonoscopy interval FIT.
The findings underscore that "positive results carried a high risk of advanced neoplasia or cancer, irrespective or prior polypectomy history," Wilson said.
Commenting on the study, William D. Chey, MD, chief of the Division of Gastroenterology & Hepatology at the University of Michigan in Ann Arbor, Michigan, noted that the study "addresses one of the biggest challenges we face as a profession, which is making sure that patients who have a positive stool test get a colonoscopy."
He noted that the low rate of just 50% of recipients of positive FITs going on to receive a colonoscopy is consistent with what is observed in other trials.
"Other data suggest that the rate might even be significantly higher -- at 70% to 80%, depending upon the population and the test," Chey told Medscape Medical News.
Reasons for the failure to receive the follow-up testing range from income restrictions (due to the high cost of a colonoscopy, especially if not covered by insurance), education, speaking a foreign language, and other factors, he said.
The relatively high rates of colon cancers detected by FIT in the study, in those with and without a prior polypectomy, along with findings from other studies "should raise questions about whether there might be a role for FIT testing in addition to colonoscopy." However, much stronger evidence would be needed, Chey noted.
In the meantime, a key issue is "how do we do a better job of making sure that individuals who have a positive FIT test get a colonoscopy," he said.
"I think a lot of this is going to come down to how it's down at the primary care level."
Chey added that in that, and any other setting, "the main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it's positive, a follow-up colonoscopy must be performed.
"Otherwise, the stool-based test is of no value."
Wilson had no disclosures to report. Chey's disclosures include consulting and/or other relationships with Ardelyx, Atmo, Biomerica, Commonwealth Diagnostics International, Corprata, Dieta, Evinature, Food Marble, Gemelli, Kiwi BioScience, Modify Health, Nestle, Phathom, Redhill, Salix/Valean, Takeda, and Vibrant.
A version of this article first appeared on Medscape.com.
Patients With a Positive FIT Fail to Get Follow-Up Colonoscopies
Patients With a Positive FIT Fail to Get Follow-Up Colonoscopies
When in the Treatment Sequence Should Metastatic CRC Be Retreated With an Anti-EGFR?
BERLIN — Re-treatment with an antiepidermal growth factor receptor (EGFR) agent is effective in patients with chemorefractory metastatic colorectal cancer (mCRC) with RAS and BRAF wild-type tumors confirmed on circulating tumor DNA (ctDNA), although the sequencing of therapy does not seem to matter, suggest overall survival results from the crossover trial PARERE.
The findings nevertheless indicate that anti-EGFR rechallenge with panitumumab may prolong progression-free survival (PFS) over the multiple kinase inhibitor regorafenib. This suggests that “the most pragmatic choice” would be to give the anti-EGFR before regorafenib, said study presenter Marco Maria Germani, MD, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy.
The caveat, however, is in patients who have an anti-EGFR interval since previously receiving the drugs of < 6 months. Those patients appeared to do better if they had regorafenib first and then anti-EGFR rechallenge.
Overall, Germani said that “since [trifluridine/tipiracil] plus bevacizumab is today the third-line standard of care” in this patient population, “anti-EGFR re-treatment might be considered after progression” on that combination.
Germani presented the research on October 18 at the European Society for Medical Oncology (ESMO) Annual Meeting 2025, which was simultaneously published in the Annals of Oncology.
Michel P. Ducreux, MD, PhD, head of the Digestive Cancer Committee at Gustave Roussy, Villejuif, France, and invited discussant for the results, said, despite the study being negative, it is “very important to continue to perform this kind of trial to evaluate the [ideal] sequence in the treatment of our patients.”
He continued that the secondary endpoints in the trial of PFS and objective response and disease control rates were “fairly in favor of the use of rechallenge before regorafenib, and in my opinion, this is really quite convincing.”
Ducreux, who was not involved in PARERE trail, also pointed to the sex difference seen in the study, which suggested that women responded much better to having anti-EGFR retreatment before regorafenib than did men.
Similar findings have been reported in a number of other trials, and previous work has suggested that there are sex differences in the pharmacokinetics of several anticancer drugs. However, while this is “very important,” he said that “we never consider it, because we are not able to really explain [it].”
Overall, he concluded that, on the basis of these results, he would agree with the notion that it is better to propose a rechallenge with anti-EGFR treatment as the fourth-line therapy in this patient population, before administering regorafenib.
Ducreux explained that, after a partial response, tumors acquire resistance to EGFR inhibitors through alterations and mutations that occur during treatment, via nongenetic mechanisms, and through treatment-induced selection for preexisting mutations.
Previous work has shown that mutations, such as in the RAS gene, are detectable early during EGFR inhibitor therapy, but that they then decay exponentially once the drugs are stopped, with the potential that tumors regain their sensitivity to them.
Germani said that this means that ctDNA-guided retreatment with anti-EGFR therapies is a “promising approach” in pretreated patients with RAS and BRAF wild-type mCRC, and that the sequencing of the drugs may be important. Indeed, the REVERCE trial showed that giving regorafenib followed by the anti-EGFR drug cetuzximab was associated with longer overall survival than the other way around in anti-EGFR medication-naive patients.
Methods and Results
For PARERE, the researchers enrolled patients aged at least 18 years with RAS and BRAF wild-type mCRC who were previously treated with a first-line anti-EGFR-containing regimen and had at least a partial response or stable disease for at least 6 months.
The patients were also required to have had at least one intervening anti-EGFR-free line of therapy, and to have previously received treatment with fluoropyrimidine, oxaliplatin, irinotecan, and anti-angiogenics. At least 4 months were required to have passed between the end of anti-EGFR administration and screening for the study.
In all, 428 patients were screened between December 2020 and December 2024, with 213 patients with RAS and BRAF wild-type mCRC, as detected on ctDNA, enrolled. They were randomized to panitumumab or regorafenib until first progression, followed by regorafenib, if they started on panitumumab, or panitumumab, if they started on regorafenib, until second progression.
The median age of the patients was 61 years among those who started on panitumumab and 64 years among those initially given regorafenib in the trial, and 63% and 57%, respectively, were male. The median number of prior lines of therapy was two in both groups, and 65% and 69%, respectively, had received pantitumumab as their first-line anti-EGFR.
Initial findings from the study presented at the 2025 ASCO Annual Meeting indicated that, after a median follow-up of 23.5 months, there was no significant difference in the median first PFS between the two treatment arms.
However, patients who started with panitumumab had a significant improvement in both the objective response and disease control rates (P < .001), as well as a signal for a potentially longer median second PFS, than those who started with regorafenib, particularly on the per-protocol analysis.
Presenting the overall survival results, Germani said that there was no significant difference between the groups on the intention-to-treat analysis, at a stratified hazard ratio of 1.13 (P = .440), or on the per-protocol analysis, at a hazard ratio of 1.07 (P = .730).
“We then ran a subgroup analysis,” he continued, “and we found out that an anti-EGFR-free interval before liquid biopsy shorter than 6 months was associated with less benefit from a panitumumab [first] sequence, which is biologically sound.”
It was also observed that women did significantly better when having panitumumab first, whereas men did not, for which “we do not have a clear biological explanation,” Germani added.
Confining the analysis to so-called “hyperselected” patients, who not only were RAS and BRAF wild type but also had no pathogenic mutations associated with anti-EGFR resistance, did not reveal any significant overall survival differences between the treatment groups.
However, Ducreux took issue with the way in which hyperselection, which is turning up more and more regularly in trials, is defined, as the choice of which mutations to include varies widely. He suggested that a consensus group be assembled to resolve this issue.
Looking more broadly, the researchers were able to show that, in this updated analysis, anti-EGFR re-treatment was superior to regorafenib regardless of the treatment sequence in terms of PFS, at 4.2 months vs 2.4 months (P = .103) when given first in the trial, and 3.9 months vs 2.7 months (P = .019) when given second in the trial, as well as in terms of objective response and disease control rates.
Adverse Events
In terms of safety, the results showed that, as expected, acneiform rash, fatigue, and hypomagnesemia were the most common adverse events associated with panitumumb, while those with regorafenib were fatigue, hand-foot skin reactions, and hypertension.
There were no notable differences in the number of patients receiving a post-study treatment nor in the post-study therapeutic choices, between the study arms.
The study was sponsored by GONO Foundation and partially supported by Amgen and Bayer. Germani declared having relationships with MSD and Amgen. Ducreux declared having relationships with Amgen, Bayer, BeiGene, Incyte, Jazz, Merck KGaA, Merck Serono, Merck Sharp & Dohme, Pierre Fabre, Roche, Servier, Keocyt, AbbVie, Abcely, Arcus, Bayer, BMS, Boehringer, GlaxoSmithKline, Sanofi, Scandion, and Zymeworks.
A version of this article first appeared on Medscape.com.
BERLIN — Re-treatment with an antiepidermal growth factor receptor (EGFR) agent is effective in patients with chemorefractory metastatic colorectal cancer (mCRC) with RAS and BRAF wild-type tumors confirmed on circulating tumor DNA (ctDNA), although the sequencing of therapy does not seem to matter, suggest overall survival results from the crossover trial PARERE.
The findings nevertheless indicate that anti-EGFR rechallenge with panitumumab may prolong progression-free survival (PFS) over the multiple kinase inhibitor regorafenib. This suggests that “the most pragmatic choice” would be to give the anti-EGFR before regorafenib, said study presenter Marco Maria Germani, MD, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy.
The caveat, however, is in patients who have an anti-EGFR interval since previously receiving the drugs of < 6 months. Those patients appeared to do better if they had regorafenib first and then anti-EGFR rechallenge.
Overall, Germani said that “since [trifluridine/tipiracil] plus bevacizumab is today the third-line standard of care” in this patient population, “anti-EGFR re-treatment might be considered after progression” on that combination.
Germani presented the research on October 18 at the European Society for Medical Oncology (ESMO) Annual Meeting 2025, which was simultaneously published in the Annals of Oncology.
Michel P. Ducreux, MD, PhD, head of the Digestive Cancer Committee at Gustave Roussy, Villejuif, France, and invited discussant for the results, said, despite the study being negative, it is “very important to continue to perform this kind of trial to evaluate the [ideal] sequence in the treatment of our patients.”
He continued that the secondary endpoints in the trial of PFS and objective response and disease control rates were “fairly in favor of the use of rechallenge before regorafenib, and in my opinion, this is really quite convincing.”
Ducreux, who was not involved in PARERE trail, also pointed to the sex difference seen in the study, which suggested that women responded much better to having anti-EGFR retreatment before regorafenib than did men.
Similar findings have been reported in a number of other trials, and previous work has suggested that there are sex differences in the pharmacokinetics of several anticancer drugs. However, while this is “very important,” he said that “we never consider it, because we are not able to really explain [it].”
Overall, he concluded that, on the basis of these results, he would agree with the notion that it is better to propose a rechallenge with anti-EGFR treatment as the fourth-line therapy in this patient population, before administering regorafenib.
Ducreux explained that, after a partial response, tumors acquire resistance to EGFR inhibitors through alterations and mutations that occur during treatment, via nongenetic mechanisms, and through treatment-induced selection for preexisting mutations.
Previous work has shown that mutations, such as in the RAS gene, are detectable early during EGFR inhibitor therapy, but that they then decay exponentially once the drugs are stopped, with the potential that tumors regain their sensitivity to them.
Germani said that this means that ctDNA-guided retreatment with anti-EGFR therapies is a “promising approach” in pretreated patients with RAS and BRAF wild-type mCRC, and that the sequencing of the drugs may be important. Indeed, the REVERCE trial showed that giving regorafenib followed by the anti-EGFR drug cetuzximab was associated with longer overall survival than the other way around in anti-EGFR medication-naive patients.
Methods and Results
For PARERE, the researchers enrolled patients aged at least 18 years with RAS and BRAF wild-type mCRC who were previously treated with a first-line anti-EGFR-containing regimen and had at least a partial response or stable disease for at least 6 months.
The patients were also required to have had at least one intervening anti-EGFR-free line of therapy, and to have previously received treatment with fluoropyrimidine, oxaliplatin, irinotecan, and anti-angiogenics. At least 4 months were required to have passed between the end of anti-EGFR administration and screening for the study.
In all, 428 patients were screened between December 2020 and December 2024, with 213 patients with RAS and BRAF wild-type mCRC, as detected on ctDNA, enrolled. They were randomized to panitumumab or regorafenib until first progression, followed by regorafenib, if they started on panitumumab, or panitumumab, if they started on regorafenib, until second progression.
The median age of the patients was 61 years among those who started on panitumumab and 64 years among those initially given regorafenib in the trial, and 63% and 57%, respectively, were male. The median number of prior lines of therapy was two in both groups, and 65% and 69%, respectively, had received pantitumumab as their first-line anti-EGFR.
Initial findings from the study presented at the 2025 ASCO Annual Meeting indicated that, after a median follow-up of 23.5 months, there was no significant difference in the median first PFS between the two treatment arms.
However, patients who started with panitumumab had a significant improvement in both the objective response and disease control rates (P < .001), as well as a signal for a potentially longer median second PFS, than those who started with regorafenib, particularly on the per-protocol analysis.
Presenting the overall survival results, Germani said that there was no significant difference between the groups on the intention-to-treat analysis, at a stratified hazard ratio of 1.13 (P = .440), or on the per-protocol analysis, at a hazard ratio of 1.07 (P = .730).
“We then ran a subgroup analysis,” he continued, “and we found out that an anti-EGFR-free interval before liquid biopsy shorter than 6 months was associated with less benefit from a panitumumab [first] sequence, which is biologically sound.”
It was also observed that women did significantly better when having panitumumab first, whereas men did not, for which “we do not have a clear biological explanation,” Germani added.
Confining the analysis to so-called “hyperselected” patients, who not only were RAS and BRAF wild type but also had no pathogenic mutations associated with anti-EGFR resistance, did not reveal any significant overall survival differences between the treatment groups.
However, Ducreux took issue with the way in which hyperselection, which is turning up more and more regularly in trials, is defined, as the choice of which mutations to include varies widely. He suggested that a consensus group be assembled to resolve this issue.
Looking more broadly, the researchers were able to show that, in this updated analysis, anti-EGFR re-treatment was superior to regorafenib regardless of the treatment sequence in terms of PFS, at 4.2 months vs 2.4 months (P = .103) when given first in the trial, and 3.9 months vs 2.7 months (P = .019) when given second in the trial, as well as in terms of objective response and disease control rates.
Adverse Events
In terms of safety, the results showed that, as expected, acneiform rash, fatigue, and hypomagnesemia were the most common adverse events associated with panitumumb, while those with regorafenib were fatigue, hand-foot skin reactions, and hypertension.
There were no notable differences in the number of patients receiving a post-study treatment nor in the post-study therapeutic choices, between the study arms.
The study was sponsored by GONO Foundation and partially supported by Amgen and Bayer. Germani declared having relationships with MSD and Amgen. Ducreux declared having relationships with Amgen, Bayer, BeiGene, Incyte, Jazz, Merck KGaA, Merck Serono, Merck Sharp & Dohme, Pierre Fabre, Roche, Servier, Keocyt, AbbVie, Abcely, Arcus, Bayer, BMS, Boehringer, GlaxoSmithKline, Sanofi, Scandion, and Zymeworks.
A version of this article first appeared on Medscape.com.
BERLIN — Re-treatment with an antiepidermal growth factor receptor (EGFR) agent is effective in patients with chemorefractory metastatic colorectal cancer (mCRC) with RAS and BRAF wild-type tumors confirmed on circulating tumor DNA (ctDNA), although the sequencing of therapy does not seem to matter, suggest overall survival results from the crossover trial PARERE.
The findings nevertheless indicate that anti-EGFR rechallenge with panitumumab may prolong progression-free survival (PFS) over the multiple kinase inhibitor regorafenib. This suggests that “the most pragmatic choice” would be to give the anti-EGFR before regorafenib, said study presenter Marco Maria Germani, MD, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy.
The caveat, however, is in patients who have an anti-EGFR interval since previously receiving the drugs of < 6 months. Those patients appeared to do better if they had regorafenib first and then anti-EGFR rechallenge.
Overall, Germani said that “since [trifluridine/tipiracil] plus bevacizumab is today the third-line standard of care” in this patient population, “anti-EGFR re-treatment might be considered after progression” on that combination.
Germani presented the research on October 18 at the European Society for Medical Oncology (ESMO) Annual Meeting 2025, which was simultaneously published in the Annals of Oncology.
Michel P. Ducreux, MD, PhD, head of the Digestive Cancer Committee at Gustave Roussy, Villejuif, France, and invited discussant for the results, said, despite the study being negative, it is “very important to continue to perform this kind of trial to evaluate the [ideal] sequence in the treatment of our patients.”
He continued that the secondary endpoints in the trial of PFS and objective response and disease control rates were “fairly in favor of the use of rechallenge before regorafenib, and in my opinion, this is really quite convincing.”
Ducreux, who was not involved in PARERE trail, also pointed to the sex difference seen in the study, which suggested that women responded much better to having anti-EGFR retreatment before regorafenib than did men.
Similar findings have been reported in a number of other trials, and previous work has suggested that there are sex differences in the pharmacokinetics of several anticancer drugs. However, while this is “very important,” he said that “we never consider it, because we are not able to really explain [it].”
Overall, he concluded that, on the basis of these results, he would agree with the notion that it is better to propose a rechallenge with anti-EGFR treatment as the fourth-line therapy in this patient population, before administering regorafenib.
Ducreux explained that, after a partial response, tumors acquire resistance to EGFR inhibitors through alterations and mutations that occur during treatment, via nongenetic mechanisms, and through treatment-induced selection for preexisting mutations.
Previous work has shown that mutations, such as in the RAS gene, are detectable early during EGFR inhibitor therapy, but that they then decay exponentially once the drugs are stopped, with the potential that tumors regain their sensitivity to them.
Germani said that this means that ctDNA-guided retreatment with anti-EGFR therapies is a “promising approach” in pretreated patients with RAS and BRAF wild-type mCRC, and that the sequencing of the drugs may be important. Indeed, the REVERCE trial showed that giving regorafenib followed by the anti-EGFR drug cetuzximab was associated with longer overall survival than the other way around in anti-EGFR medication-naive patients.
Methods and Results
For PARERE, the researchers enrolled patients aged at least 18 years with RAS and BRAF wild-type mCRC who were previously treated with a first-line anti-EGFR-containing regimen and had at least a partial response or stable disease for at least 6 months.
The patients were also required to have had at least one intervening anti-EGFR-free line of therapy, and to have previously received treatment with fluoropyrimidine, oxaliplatin, irinotecan, and anti-angiogenics. At least 4 months were required to have passed between the end of anti-EGFR administration and screening for the study.
In all, 428 patients were screened between December 2020 and December 2024, with 213 patients with RAS and BRAF wild-type mCRC, as detected on ctDNA, enrolled. They were randomized to panitumumab or regorafenib until first progression, followed by regorafenib, if they started on panitumumab, or panitumumab, if they started on regorafenib, until second progression.
The median age of the patients was 61 years among those who started on panitumumab and 64 years among those initially given regorafenib in the trial, and 63% and 57%, respectively, were male. The median number of prior lines of therapy was two in both groups, and 65% and 69%, respectively, had received pantitumumab as their first-line anti-EGFR.
Initial findings from the study presented at the 2025 ASCO Annual Meeting indicated that, after a median follow-up of 23.5 months, there was no significant difference in the median first PFS between the two treatment arms.
However, patients who started with panitumumab had a significant improvement in both the objective response and disease control rates (P < .001), as well as a signal for a potentially longer median second PFS, than those who started with regorafenib, particularly on the per-protocol analysis.
Presenting the overall survival results, Germani said that there was no significant difference between the groups on the intention-to-treat analysis, at a stratified hazard ratio of 1.13 (P = .440), or on the per-protocol analysis, at a hazard ratio of 1.07 (P = .730).
“We then ran a subgroup analysis,” he continued, “and we found out that an anti-EGFR-free interval before liquid biopsy shorter than 6 months was associated with less benefit from a panitumumab [first] sequence, which is biologically sound.”
It was also observed that women did significantly better when having panitumumab first, whereas men did not, for which “we do not have a clear biological explanation,” Germani added.
Confining the analysis to so-called “hyperselected” patients, who not only were RAS and BRAF wild type but also had no pathogenic mutations associated with anti-EGFR resistance, did not reveal any significant overall survival differences between the treatment groups.
However, Ducreux took issue with the way in which hyperselection, which is turning up more and more regularly in trials, is defined, as the choice of which mutations to include varies widely. He suggested that a consensus group be assembled to resolve this issue.
Looking more broadly, the researchers were able to show that, in this updated analysis, anti-EGFR re-treatment was superior to regorafenib regardless of the treatment sequence in terms of PFS, at 4.2 months vs 2.4 months (P = .103) when given first in the trial, and 3.9 months vs 2.7 months (P = .019) when given second in the trial, as well as in terms of objective response and disease control rates.
Adverse Events
In terms of safety, the results showed that, as expected, acneiform rash, fatigue, and hypomagnesemia were the most common adverse events associated with panitumumb, while those with regorafenib were fatigue, hand-foot skin reactions, and hypertension.
There were no notable differences in the number of patients receiving a post-study treatment nor in the post-study therapeutic choices, between the study arms.
The study was sponsored by GONO Foundation and partially supported by Amgen and Bayer. Germani declared having relationships with MSD and Amgen. Ducreux declared having relationships with Amgen, Bayer, BeiGene, Incyte, Jazz, Merck KGaA, Merck Serono, Merck Sharp & Dohme, Pierre Fabre, Roche, Servier, Keocyt, AbbVie, Abcely, Arcus, Bayer, BMS, Boehringer, GlaxoSmithKline, Sanofi, Scandion, and Zymeworks.
A version of this article first appeared on Medscape.com.
FROM ENDO 2025
Shifting Demographics: A Temporal Analysis of the Alarming Rise in Rectal Adenocarcinoma Among Young Adults
Background
Rectal adenocarcinoma has long been associated with older adults, with routine screening typically beginning at age 45 or older. However, recent data reveal a concerning rise in rectal cancer incidence among adults under 40. These early-onset cases often present at later stages and may have distinct biological features. While some research attributes this trend to genetic or environmental factors, the contribution of socioeconomic disparities and healthcare access has not been fully explored. Identifying these influences is essential to shaping targeted prevention and early detection strategies for younger populations.
Objective
To evaluate temporal trends in rectal adenocarcinoma among young adults and assess demographic and socioeconomic predictors of early-onset diagnosis.
Methods
Data were drawn from the National Cancer Database (NCDB) for patients diagnosed with rectal adenocarcinoma from 2004 to 2022. Among 440,316 cases, 17,842 (4.1%) occurred in individuals under 40. Linear regression assessed temporal trends, while logistic regression evaluated associations between early-onset diagnosis and variables including sex, race, insurance status, income level, Charlson-Deyo comorbidity score, and tumor stage. Statistical significance was defined as α = 0.05.
Results
The number of young adults diagnosed rose from 424 in 2004 to 937 in 2022—an increase of over 120%. Each year was associated with a 1.7% rise in odds of early diagnosis (OR = 1.017, p < 0.001). Male patients had 24.7% higher odds (OR = 1.247, p < 0.001), and Black patients had 59.3% higher odds compared to White patients (OR = 1.593, p < 0.001). Non-private insurance was linked to a 41.6% decrease in early diagnosis (OR = 0.584, p < 0.001). Income level was not significant (p = 0.426). Lower Charlson-Deyo scores and higher tumor stages were also associated with early-onset cases.
Conclusions
Rectal adenocarcinoma is increasingly affecting younger adults, with significant associations across demographic and insurance variables. These findings call for improved awareness, early diagnostic strategies, and further research into underlying causes to mitigate this growing public health concern.
Background
Rectal adenocarcinoma has long been associated with older adults, with routine screening typically beginning at age 45 or older. However, recent data reveal a concerning rise in rectal cancer incidence among adults under 40. These early-onset cases often present at later stages and may have distinct biological features. While some research attributes this trend to genetic or environmental factors, the contribution of socioeconomic disparities and healthcare access has not been fully explored. Identifying these influences is essential to shaping targeted prevention and early detection strategies for younger populations.
Objective
To evaluate temporal trends in rectal adenocarcinoma among young adults and assess demographic and socioeconomic predictors of early-onset diagnosis.
Methods
Data were drawn from the National Cancer Database (NCDB) for patients diagnosed with rectal adenocarcinoma from 2004 to 2022. Among 440,316 cases, 17,842 (4.1%) occurred in individuals under 40. Linear regression assessed temporal trends, while logistic regression evaluated associations between early-onset diagnosis and variables including sex, race, insurance status, income level, Charlson-Deyo comorbidity score, and tumor stage. Statistical significance was defined as α = 0.05.
Results
The number of young adults diagnosed rose from 424 in 2004 to 937 in 2022—an increase of over 120%. Each year was associated with a 1.7% rise in odds of early diagnosis (OR = 1.017, p < 0.001). Male patients had 24.7% higher odds (OR = 1.247, p < 0.001), and Black patients had 59.3% higher odds compared to White patients (OR = 1.593, p < 0.001). Non-private insurance was linked to a 41.6% decrease in early diagnosis (OR = 0.584, p < 0.001). Income level was not significant (p = 0.426). Lower Charlson-Deyo scores and higher tumor stages were also associated with early-onset cases.
Conclusions
Rectal adenocarcinoma is increasingly affecting younger adults, with significant associations across demographic and insurance variables. These findings call for improved awareness, early diagnostic strategies, and further research into underlying causes to mitigate this growing public health concern.
Background
Rectal adenocarcinoma has long been associated with older adults, with routine screening typically beginning at age 45 or older. However, recent data reveal a concerning rise in rectal cancer incidence among adults under 40. These early-onset cases often present at later stages and may have distinct biological features. While some research attributes this trend to genetic or environmental factors, the contribution of socioeconomic disparities and healthcare access has not been fully explored. Identifying these influences is essential to shaping targeted prevention and early detection strategies for younger populations.
Objective
To evaluate temporal trends in rectal adenocarcinoma among young adults and assess demographic and socioeconomic predictors of early-onset diagnosis.
Methods
Data were drawn from the National Cancer Database (NCDB) for patients diagnosed with rectal adenocarcinoma from 2004 to 2022. Among 440,316 cases, 17,842 (4.1%) occurred in individuals under 40. Linear regression assessed temporal trends, while logistic regression evaluated associations between early-onset diagnosis and variables including sex, race, insurance status, income level, Charlson-Deyo comorbidity score, and tumor stage. Statistical significance was defined as α = 0.05.
Results
The number of young adults diagnosed rose from 424 in 2004 to 937 in 2022—an increase of over 120%. Each year was associated with a 1.7% rise in odds of early diagnosis (OR = 1.017, p < 0.001). Male patients had 24.7% higher odds (OR = 1.247, p < 0.001), and Black patients had 59.3% higher odds compared to White patients (OR = 1.593, p < 0.001). Non-private insurance was linked to a 41.6% decrease in early diagnosis (OR = 0.584, p < 0.001). Income level was not significant (p = 0.426). Lower Charlson-Deyo scores and higher tumor stages were also associated with early-onset cases.
Conclusions
Rectal adenocarcinoma is increasingly affecting younger adults, with significant associations across demographic and insurance variables. These findings call for improved awareness, early diagnostic strategies, and further research into underlying causes to mitigate this growing public health concern.
An Unusual Metastasis of Anal Squamous Cell Carcinoma
Background
Anal squamous cell carcinoma is a rare cancer which usually has locoregional spread. We report a case of distant metastasis of primary anal squamous cell carcinoma to the posterior mediastinal lymph node without lung involvement.
Case Presentation
A 63-year-old female presented with a painful anal mass, bleeding, and fluid leakage for around six months. The patient was found to have a near-circumferential fungating anal mass with bilateral inguinal lymphadenopathy. MR imaging revealed an 8.7 x 5.9 cm anal mass extending beyond the mesorectal fascia, with lymphadenopathy involving inguinal, pelvic sidewall, and iliac regions. A biopsy of the mass confirmed anal squamous cell carcinoma (ASCC). Initial treatment included diverting colostomy followed by definitive chemoradiotherapy with Mitomycin and 5-Fluorouracil. Colonoscopy post-treatment revealed tubular adenomas and a hyperplastic polyp, with no malignancy detected. The patient demonstrated a strong therapeutic response, with resolution of the anal mass and improved symptoms. However, one year later, new FDG-avid mediastinal lymph node were detected on the CT/PET scan with no pulmonary involvement. Metastatic ASCC of the Mediastinal lymph node was confirmed by biopsy. Salvage chemotherapy with Carboplatin and Paclitaxel every three weeks for six cycles achieved complete resolution of metastases.
Conclusions
This case underscores the importance of a multidisciplinary approach in managing advanced ASCC and highlights the efficacy of salvage chemotherapy in addressing metastases. Close monitoring of disease progression following surgery and chemotherapy is crucial due to the risk of recurrence.
Background
Anal squamous cell carcinoma is a rare cancer which usually has locoregional spread. We report a case of distant metastasis of primary anal squamous cell carcinoma to the posterior mediastinal lymph node without lung involvement.
Case Presentation
A 63-year-old female presented with a painful anal mass, bleeding, and fluid leakage for around six months. The patient was found to have a near-circumferential fungating anal mass with bilateral inguinal lymphadenopathy. MR imaging revealed an 8.7 x 5.9 cm anal mass extending beyond the mesorectal fascia, with lymphadenopathy involving inguinal, pelvic sidewall, and iliac regions. A biopsy of the mass confirmed anal squamous cell carcinoma (ASCC). Initial treatment included diverting colostomy followed by definitive chemoradiotherapy with Mitomycin and 5-Fluorouracil. Colonoscopy post-treatment revealed tubular adenomas and a hyperplastic polyp, with no malignancy detected. The patient demonstrated a strong therapeutic response, with resolution of the anal mass and improved symptoms. However, one year later, new FDG-avid mediastinal lymph node were detected on the CT/PET scan with no pulmonary involvement. Metastatic ASCC of the Mediastinal lymph node was confirmed by biopsy. Salvage chemotherapy with Carboplatin and Paclitaxel every three weeks for six cycles achieved complete resolution of metastases.
Conclusions
This case underscores the importance of a multidisciplinary approach in managing advanced ASCC and highlights the efficacy of salvage chemotherapy in addressing metastases. Close monitoring of disease progression following surgery and chemotherapy is crucial due to the risk of recurrence.
Background
Anal squamous cell carcinoma is a rare cancer which usually has locoregional spread. We report a case of distant metastasis of primary anal squamous cell carcinoma to the posterior mediastinal lymph node without lung involvement.
Case Presentation
A 63-year-old female presented with a painful anal mass, bleeding, and fluid leakage for around six months. The patient was found to have a near-circumferential fungating anal mass with bilateral inguinal lymphadenopathy. MR imaging revealed an 8.7 x 5.9 cm anal mass extending beyond the mesorectal fascia, with lymphadenopathy involving inguinal, pelvic sidewall, and iliac regions. A biopsy of the mass confirmed anal squamous cell carcinoma (ASCC). Initial treatment included diverting colostomy followed by definitive chemoradiotherapy with Mitomycin and 5-Fluorouracil. Colonoscopy post-treatment revealed tubular adenomas and a hyperplastic polyp, with no malignancy detected. The patient demonstrated a strong therapeutic response, with resolution of the anal mass and improved symptoms. However, one year later, new FDG-avid mediastinal lymph node were detected on the CT/PET scan with no pulmonary involvement. Metastatic ASCC of the Mediastinal lymph node was confirmed by biopsy. Salvage chemotherapy with Carboplatin and Paclitaxel every three weeks for six cycles achieved complete resolution of metastases.
Conclusions
This case underscores the importance of a multidisciplinary approach in managing advanced ASCC and highlights the efficacy of salvage chemotherapy in addressing metastases. Close monitoring of disease progression following surgery and chemotherapy is crucial due to the risk of recurrence.